
Although the vast majority of cases are preventable, blood clots are a serious public health problem that kills hundreds of thousands of adults each year.
In the U.S. alone, up to 300,000 people die each year from blood clot conditions called deep vein thrombosis (DVT), formed when blood thickens and clumps together, then travels and causes complications, such as a stroke.
While sometimes blood clots cause, symptoms noticeable enough for a patient to visit the doctor, such as leg pain, symptoms of deep vein thrombosis can also go unnoticed, which can be very dangerous.
If thrombosis runs in your family, you’re over the age of 60, or you have a family history of other heart and vascular complications, you’re at a higher risk for developing DVT.
Your health is still within your control; however — since research shows that other lifestyle-related risk factors significantly impact your chances of developing DVT,
including being overweight or obese, inactivity, smoking, and taking birth control or hormone replacement drugs.
Improving your diet, staying active, losing weight, and controlling your blood pressure are essential steps in naturally preventing clots and stopping them from returning.
What Is Deep Vein Thrombosis (DVT)?
Thrombosis is the term for a medical condition that occurs when a blood clot (called a thrombus) forms in an artery or vein.
Deep vein thrombosis, often just called DVT for short, is precisely the kind of thrombosis caused when a blood clot develops in a deep vein, most often in the lower leg, thigh, or pelvis.
On the other hand, when a clot forms in a vein that’s closer to the surface of your skin, this type of thrombosis is called “superficial thrombosis.”
Compared to superficial thrombosis, DVT is considered to be much more severe and complicated.
Superficial thrombosis usually doesn’t cause life-threatening complications (such as a stroke) and often clears on its own, while DVT clots pose more risks.
A deep vein thrombosis clot can detach from the original site where it developed and travel through the bloodstream to other areas of the body, including your lungs or brain (this is called an embolus).
When that happens, either a condition called a pulmonary embolism (PE) can develop in your lungs, or you might even suffer from a stroke if blood supply is cut off to your brain.
This is the most significant risk associated with DVT: a clot traveling and forming a blockage in essential blood vessels, which at times is deadly.
Pulmonary embolism is commonly fatal and occurs when a clot breaks free and blocks the arteries of the lungs.
DVT/PE often occur together, and when they do this is called venous thromboembolism.
Estimates from the Centers for Disease Control and Prevention reveal that between 10 percent and 30 percent of people with venous thromboembolism die within one month of diagnosis, and many die suddenly without little to no warning.
Deep Vein Thrombosis Causes
Blood clots are made up of clusters of blood cells called platelets, which every person has and relies on to survive.
Platelets are responsible for helping blood to clot within an injured or damaged artery/vein, so you don’t bleed too much whenever you’re hurt, scraped, bruised, or operated on.
Platelets stop excess bleeding and help repair damaged blood cells along with a network of other red blood cells and a type of protein called fibrin.
However, this process can also sometimes lead to blood clot formation, at times causing symptoms and serious complications.
Not everyone with a clot experiences any noticeable symptoms at all or has any idea that he or she has developed one —
however, the clot itself usually still causes inflammation, swelling, and localized problems internally, at the site where it forms.
Risk factors that put you at a higher risk for DVT include: (3)
- Being over 60: Older adults are more likely to have DVT than younger adults. Those over 75 are at the highest risk, especially if they’re overweight.
- Genetic factors: Certain inherited traits can lead to genetic blood-clotting disorders or the production of too many platelets. This causes blood to clot too quickly and makes clot formation more likely. The good news is that having DVT in your family doesn’t necessarily mean that you’ll get it yourself since genetic predisposition usually needs to be combined with other risk factors for a clot to form.
- A sedentary lifestyle: Being inactive for long periods, especially being put on bed rest for an extended period, can contribute to blood pooling and clotting. Other lifestyle habits or scenarios that might help to thrombosis include avoiding exercise, long plane or car rides, sitting at a desk all day, watching TV for many hours, and immobilization after surgery, an injury, or another health condition. Research shows that people who have recently suffered from injuries or surgeries that stop them from walking and lead them to be more sedentary are at a higher risk of having DVT.
- A history of a heart attack or stroke: People who have had a heart attack, stroke, or heart disease are more likely to have clots than those without any history of cardiovascular problems. Those who have had injuries to veins, such as the type that can be caused by some surgical procedures or even traumatic impacts, can also develop clots more easily.
- Being overweight: Although it’s not exactly clear why, being very overweight or obese has been associated with a higher risk for blood clots, possibly because of how excess fat tissue increases estrogen levels. Estrogen stored in fatty tissue can contribute to clot formation, inflammation, and other problems that can trigger DVT.
- Pregnancy: Women seem to have a higher risk of developing clots during pregnancy and right after giving birth. Reasons for this include producing extra blood to support the fetus, more pressure being applied to veins, changes in blood pressure, and weight gain. A scary finding is that pulmonary embolism (a clot traveling to the lungs) is one of the leading causes of maternal death during birth.
- A history of cancer and other conditions: Studies have found that a history of certain types of cancer (especially lung, pancreatic, breast, and ovarian cancers) can increase clotting.
- Smoking and drug use: All of the risk factors described above for deep vein thrombosis are made worse when you smoke cigarettes, use other tobacco products, or use recreational drugs. Tobacco is even riskier when combined with medications that affect blood flow and hormone levels (such as estrogen).
- Menopause and hormonal changes: Some research shows that changes in estrogen, including increased estrogen due to taking birth control pills or hormone replacement therapy drugs, can increase blood clotting and cause various heart complications. Menopausal women seeking drugs to replace estrogen are also at a higher risk if they smoke, are overweight and don’t exercise.
Signs and Symptoms of Deep Vein Thrombosis
Although DVT doesn’t always cause symptoms, some people experience the following: (4)
- Skin redness, warmth, and swelling around the affected area (including the leg or pelvis). Sometimes the skin looks discolored and red, or dark patches appear.
- Pain and tenderness near the clot site. This might develop in only one leg or both and spread up the legs from the clot location.
- Difficulty walking or moving regularly.
- Sometimes scaling or ulcers form in the affected part of the body.
Symptoms of a blood clot in your leg might be an indication of where a lump is forming, although not always.
According to the National Heart, Lung, and Blood Institute, blood clots in the thighs are more likely to break off and cause complications than blood clots in the lower legs or other parts of the body.
If you suspect you have a clot in one of your thighs, let your doctor know right away and keep a close lookout for other symptoms.
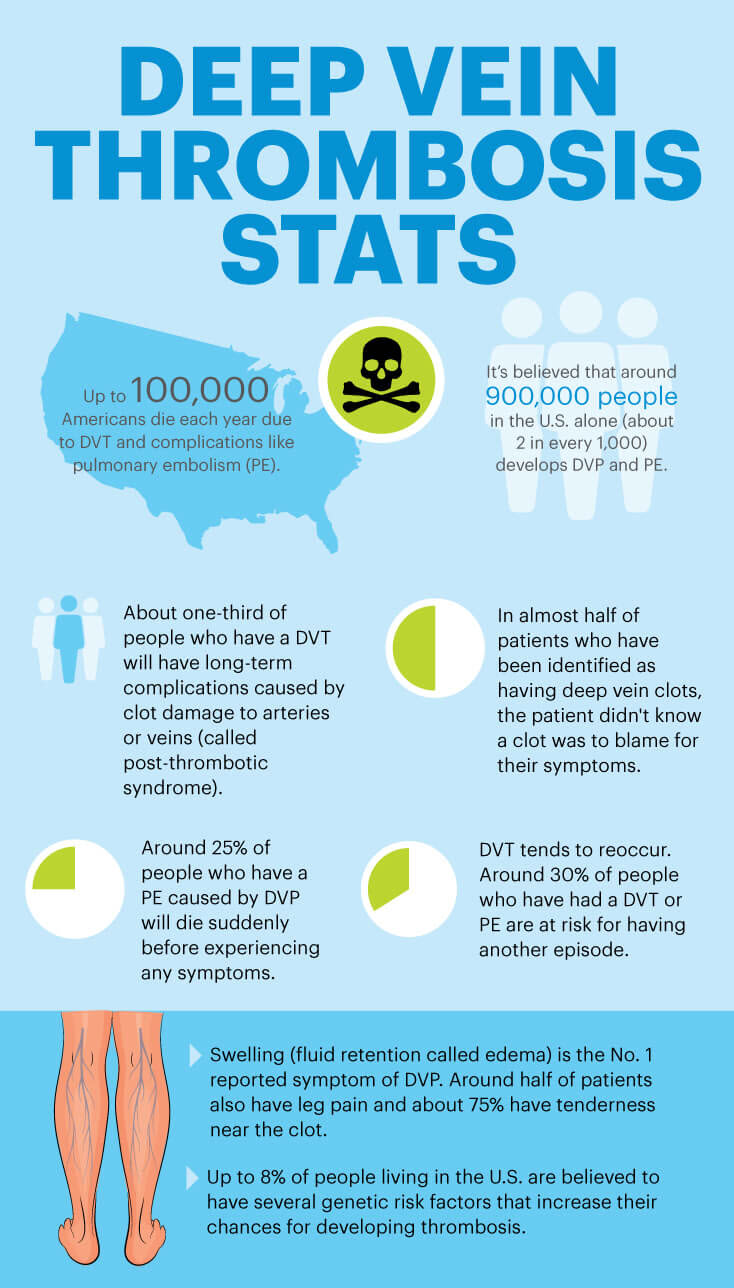
In-depth Vein Thrombosis Facts and Statistics
- Up to 100,000 Americans die each year due to deep vein thrombosis and complications like pulmonary embolism.
- It’s believed that around 900,000 people in the U.S. alone (about two in every 1,000) develops DVP and PE.
- About one-third of people who have a DVT will have long-term complications caused by clot damage to arteries or veins (called post-thrombotic syndrome). (6)
- Around 25 percent of people who have a PE caused by DVP die suddenly before experiencing any symptoms.
- DVT tends to reoccur. Around 30 percent of people who have had a DVT or PE are at risk of having another episode.
- Up to 8 percent of people living in the U.S. are believed to have several genetic risk factors that increase their chances of developing thrombosis.
- Swelling (fluid retention called edema) is the No. 1 reported symptom of DVP. Around half of the patients also have leg pain, and about 75 percent have tenderness near the clot. (7)
- In almost half of the patients who have been identified as having deep vein clots, the patient didn’t know a lump was to blame for their symptoms.
Conventional Treatment for Deep Vein Thrombosis Symptoms
The traditional approach of treatment to resolving DVT includes: (8)
- Prescribing blood-thinning drugs (such as anticoagulants called heparin, Xarelto, or warfarin) and breaking up clots using medications such as Coumadin.
- Thrombolytic drugs are used to resolve clots and stop them from traveling, where they can contribute to pulmonary embolism.
- For people who can’t take blood thinners, sometimes a vena cava filter is used to catch a clot before it reaches the lungs or brain.
- Most doctors usually also recommend a change in someone’s lifestyle, including quitting smoking and starting to exercise.
Treatment depends on the individual case, along with someone’s personal history of other medical problems.
Unfortunately, under many doctors’ orders, many people (especially those with a history of vascular problems or injury that leaves them less active) remain on medications that are used to treat DVT for their entire lives.
Blood-thinning medications like Xarelto can cause many different side effects, including bleeding complications that can sometimes be severe and even life-threatening.
Women who are pregnant also cannot take warfarin, since it’s been tied to congenital disabilities.
So taking these adverse effects into account, it’s essential to weigh the pros and cons of taking any blood-thinning drugs and do all you can to control DVT symptoms naturally.
If you do use medications to help treat your DVT, talk to your doctor about limiting your use to one to two months or less, using the minimum dose.
Also, make sure to avoid taking other drugs at the same time as blood thinners that can cause adverse side effects, including aspirin, Advil, or ibuprofen.
Natural Treatments for Deep Vein Thrombosis
1. Exercise and Move More
Leading a sedentary lifestyle, including sitting still for extended periods at a desk or elsewhere, can make you more likely to develop DVT.
The best type of exercise plan for keeping your heart and veins healthy is one that combines aerobic exercise (like running, HIIT workouts, or cycling) with resistance/strength-training moves and also stretching for flexibility.
Incorporate exercises to strengthen knees and legs, such as squats, walking, and lunges, if you have a history of clots.
Make sure to clear with your doctor that you’re ready to exercise before starting if you recently had a clot identified.
In addition to starting a regular exercise program, take breaks regularly from sitting and make sure to stretch.
For example, if you’re taking a long car or plane trip, make a point to get up at least every hour (ideally even more often if you’re at work, such as every 20 minutes) to take a break.
Sneak more exercise into your day with exercise hacks by building short break periods in your routine, so you can walk, move or stretch your legs to keep blood flowing.
If you’re healing from surgery or an injury, get up and start moving as soon as it’s safe to.
2. Switch Your Medications
Some medicines and disorders increase your risk for blood clots and can contribute to DVT.
These include hormone replacement drugs (usually used by menopausal or postmenopausal women), birth control pills, medications to control blood pressure, and cancer treatment drugs.
It’s a good idea to check with your doctor regularly to see if your medications can be lowered or if they might be contributing to any problems.
If you do decide to take blood-thinning drugs (Coumadin or Jantoven, for example), your doctor will likely want to monitor you to make sure your dose is not too high or used for too long.

3. Eat a Healthy Diet
Sticking to a healthier diet as you get older is crucial for managing your weight, controlling your blood pressure, and maintaining a healthy cardiovascular system.
Foods that are high in vitamin K, potassium, and magnesium are especially beneficial for regulating blood flow.
Green leafy vegetables, cruciferous veggies, avocado, sweet potatoes, and bananas are high in these nutrients.
However, keep in mind that vitamin K can interact with blood-thinning drugs, so make sure you’re being monitored if you’ve been prescribed these.
You also want to be sure you’re drinking plenty of water and other hydrating liquids — just stay away from added sugar and too much alcohol or caffeine.
It’s also helpful to include specific herbal treatments and supplements in your treatment or prevention plan to boost recovery and heart health.
Foods, herbs, and supplements that can have natural anticoagulant and anti-inflammatory effects include:
- Foods with vitamin E and vitamin D: found in fruits, veggies, cage-free eggs and certain types of mushrooms
- Spices and herbs, including garlic, turmeric, oregano, cayenne, and ginger
- Real dark cocoa/chocolate
- Evening primrose oil
- Fruits such as papaya, berries, and pineapple
- Raw honey
- Vinegar
- Green tea
- Fish oil and omega-3 fatty acids
4. Quit Smoking
Smoking cigarettes or using electronic cigarettes and other tobacco products are all severe risk factors for developing thrombosis, especially when combined with other risk factors like being overweight.
Quit as soon as you can with help from things like joining a support group, trying hypnosis or meditation geared toward overcoming addictions, or talking to your doctor about other ways to wean yourself off effectively.
5. Use Compression Stockings
Wearing compression stockings can help lower pressure, swelling, and pain in the affected area where a clot has formed.
Keeping the affected area raised and applying moist heat where it hurts can also help you heal.
Compression is also used because reduced pressure lowers the chances of developing another clot in the future, and it might help you start being more active earlier on.
Typically, a stocking is worn on the leg that reaches from your foot up to about your knee.
These stockings can be bought online or given to you by your doctor.
You can take off the stocking when exercising or showering and use it along with other natural remedies to control pain, such as essential oils, stretching, and massaging.
Precautions About Treating DVT
Deep vein thrombosis should be taken very seriously if you start to experience any signs or symptoms of pulmonary embolism.
This condition can damage the lungs and other organs in the body and even cause death,
so always contact your doctor right away if you notice sudden shortness of breath, chest pains, dizziness, a fast heartbeat, or coughing blood.
Although there are ways to help prevent DVT naturally, still be sure to take your medications as your doctor has prescribed them.
Don’t change medication dosages without being monitored since this can cause side effects.
Final Thoughts on Deep Vein Thrombosis
- Deep vein thrombosis occurred when a blood clot forms in a vein located deep inside your body, usually within your leg.
- DVT can be fatal due to a clot traveling and causing lung complications or a stroke.
- Symptoms of DVT include tenderness and pain in the legs, swelling, and redness.
- Natural treatments and prevention for DVT include exercising, eating an anti-inflammatory diet, adjusting your medications, losing weight, quitting smoking, and avoiding the use of estrogen-containing drugs.







