
Discover 9 popular drug classes, from allergy meds to Parkinson’s drugs, that emerging research links to increased risk of dementia and cognitive decline
As soon as you’re taking a prescription medication, weighing the risks as well as benefits is a necessity. One crucial factor to consider is the potential impact on cognitive function and brain health.
Emerging research is uncovering worrisome connections between certain classes of drugs, known as anticholinergics, and an increased risk of dementia as well as memory loss. This drug class includes common medications for conditions like allergies, insomnia, incontinence, and more.
A groundbreaking study published in JAMA Neurology used advanced brain imaging techniques to demonstrate how anticholinergic drugs can lower brain metabolism and accelerate brain atrophy. These findings build upon previous research that has linked long-term use of anticholinergic medications to a heightened risk of developing dementia.
Here are 9 popular drug classes that may contribute to memory loss and cognitive decline, along with some natural alternatives to consider:
1. Incontinence Drugs
Generic Names: darifenacin, oxybutynin, tolterodine, flavoxate
Natural Options:
- Pelvic floor muscle exercises like Kegels
- Bladder training techniques to regain control
- Nutrient-rich foods high in vitamin C and beta-cryptoxanthin
2. Muscle Relaxants
Generic Names: cyclobenzaprine, dicyclomine, orphenadrine
Natural Options:
- Massage therapy
- Magnesium supplements
3. Narcotic Painkillers
Generic Names: meperidine
Natural Options:
- Dry needling
- Cryotherapy
- Chiropractic care
- Essential oils
4. Anti-Seizure Drugs
Generic Names: carbamazepine, oxcarbazepine
Natural Alternatives:
- Identifying and managing seizure triggers
- Ketogenic diet
5. Parkinson’s Medications
Generic Names: benztropine, procyclidine, trihexyphenidyl, amantadine
Natural Alternatives:
- Deep brain stimulation
- Exercise programs
- Acupuncture
6. Tricyclic Antidepressants
Generic Names: amitriptyline, amoxapine, clomipramine, desipramine, doxepin, imipramine, nortriptyline, trimipramine
Natural Alternatives:
- Lifestyle changes like exercise
- Nutritional supplements like St. John’s Wort
7. Antipsychotic Drugs
Generic Names: clozapine, olanzapine, perphenazine, quetiapine, thioridazine, trifluoperazine, loxapine, methotrimeprazine, molindone, pimozide
Natural Alternatives:
- Community-based recovery models
- Supplements like omega-3s, l-lysine, sarcosine
- Acupuncture
8. Allergy Medications
Generic Names: carbinoxamine, chlorpheniramine, clemastine, diphenhydramine, hydroxyzine, promethazine, cyproheptadine
Natural Alternatives:
- Raw, local honey
- Neti pots
- Essential oils
- Bone broth
- Probiotics
9. Motion Sickness Drugs
Generic Names: dimenhydrinate, diphenhydramine, meclizine, promethazine, scopolamine
Natural Alternatives:
- Ginger supplements
- 5-HTP and magnesium
- Aromatherapy with peppermint or lavender
Drugs Linked to Dementia and Memory Loss
Many people are unaware that certain commonly prescribed medications may increase the risk of developing dementia and memory loss. Recent research has highlighted the potential dangers of specific drug classes, prompting healthcare professionals to advise caution when using these medications.
Understanding the connection between these drugs and cognitive decline is crucial for making informed decisions about your health.
Reference: For a comprehensive list of medications and their cognitive effects, visit the Alzheimer’s Association.
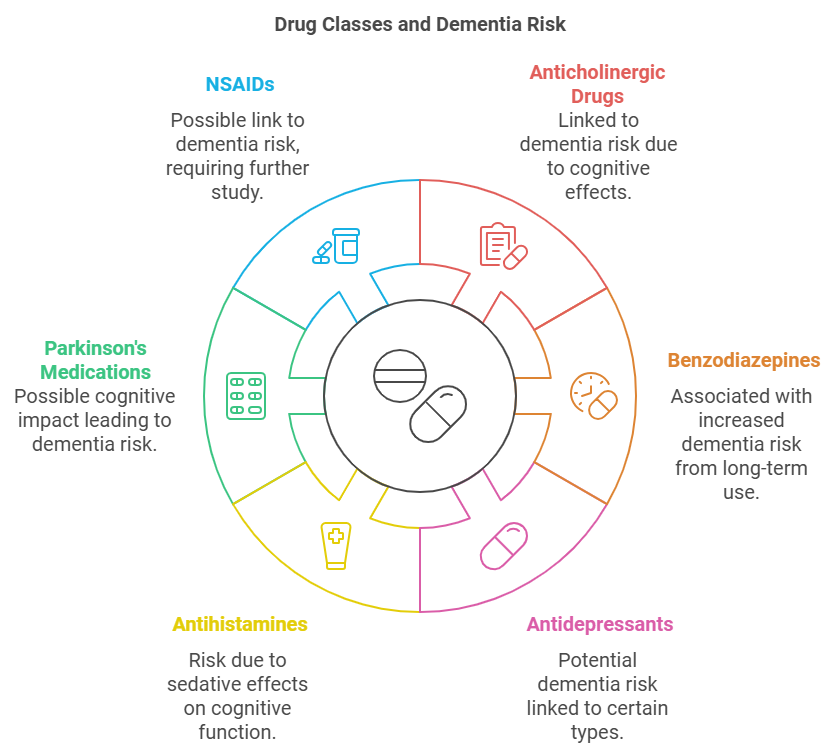
Classes of Drugs Linked to Dementia
Research has identified several classes of drugs associated with an increased risk of dementia and memory loss. Notably, anticholinergic drugs have been the focus of many studies due to their impact on neurotransmitters in the brain.
Anticholinergic medications work by blocking acetylcholine, a neurotransmitter crucial for memory and learning. These drugs are commonly prescribed for conditions such as overactive bladder, depression, and allergies. Examples include tricyclic antidepressants, antimuscarinics, and certain antihistamines.
Benzodiazepines, often prescribed for anxiety and insomnia, have also been linked to cognitive decline. These medications can cause short-term memory loss and have sedative effects, which may contribute to long-term brain health issues.
Mechanisms of Drug Impact on Cognitive Health
Understanding how these drugs affect the brain is essential. Anticholinergic drugs interfere with acetylcholine, leading to disruptions in cognitive functions. Benzodiazepines enhance the effect of gamma-aminobutyric acid (GABA), a neurotransmitter that inhibits brain activity, potentially causing chemical dependency and cognitive deficits.
Additionally, older adults metabolize drugs differently due to changes in kidney and liver function, decreased muscle mass, and increased body fat. These factors can lead to higher concentrations of medications in the body, increasing the risk of adverse effects on the brain.
Research Findings on Drug-Dementia Links
Multiple studies have investigated the potential connection between certain medications and an increased risk of dementia. One significant study published in JAMA Internal Medicine analyzed the medical records of thousands of patients over a decade. The researchers found that individuals with a higher cumulative dose of anticholinergic drugs had a substantially increased risk of developing dementia compared to those who did not use these medications.
Another notable study based on data from the Quebec Health Insurance Program, examining prescription records and dementia diagnoses. The findings suggested a dose-response relationship, where higher doses and prolonged use of anticholinergic medications correlated with greater dementia risk.
These observational studies, while not establishing causation, highlight a concerning association that warrants attention. Confounding factors, such as underlying health conditions and lifestyle choices, can influence results. However, the consistency across various research efforts strengthens the argument for cautious use of these medications, especially among older adults.
Alternatives to Dementia-Linked Medications
Exploring alternative treatments can reduce reliance on medications associated with cognitive risks. Non-pharmacological approaches, such as cognitive behavioral therapy (CBT) for depression and anxiety, may offer benefits without the associated risks.
In cases of urinary incontinence, pelvic floor muscle exercises (Kegel exercises) can be effective. For allergies, newer antihistamines with lower anticholinergic activity are preferable. Always consult with a healthcare provider before making changes to your medication regimen.
For managing allergies, newer generation antihistamines like loratadine (Claritin) and cetirizine (Zyrtec) have less anticholinergic activity and are less likely to affect cognitive function. In treating overactive bladder, non-drug therapies such as bladder training exercises and dietary adjustments may offer relief.
Guidance for Patients on Dementia-Linked Drugs
If you’re currently taking medications that may be linked to dementia, it’s crucial to discuss your concerns with your primary care doctor. Do not stop taking prescribed medications without medical advice, as abrupt changes can have serious health implications.
Your healthcare provider can assess the potential benefits and harms of your medications, considering factors like dosage, duration, and your overall health. They may suggest alternative treatments or adjust dosages to mitigate risks.
Communication with healthcare providers is essential. Schedule a comprehensive medication review with your doctor or pharmacist to assess all prescription and over-the-counter drugs you are taking. They can help identify medications with anticholinergic properties and suggest safer alternatives.
Mechanisms of Drug Impact on Cognitive Health
Understanding how these drugs affect the brain is essential. Anticholinergic drugs interfere with acetylcholine, leading to disruptions in cognitive functions. Benzodiazepines enhance the effect of gamma-aminobutyric acid (GABA), a neurotransmitter that inhibits brain activity, potentially causing chemical dependency and cognitive deficits.
Additionally, older adults metabolize drugs differently due to changes in kidney and liver function, decreased muscle mass, and increased body fat. These factors can lead to higher concentrations of medications in the body, increasing the risk of adverse effects on the brain.
Frequently Asked Questions (FAQ)
What are anticholinergic drugs, and why are they linked to dementia?
Anticholinergic drugs block the action of acetylcholine, a neurotransmitter important for memory and learning. Long-term use of these drugs has been associated with an increased risk of dementia due to their impact on crucial brain cells.
Should I stop taking my medication if it’s linked to dementia?
No, you should not stop taking any prescribed medication without consulting your healthcare provider. Abruptly stopping medication can have adverse effects. Discuss your concerns with your doctor to determine the best course of action.
Are over-the-counter medications also linked to memory loss?
Some over-the-counter medications, particularly certain antihistamines like diphenhydramine (Benadryl), have anticholinergic properties and may contribute to memory loss. Always read labels and consult a pharmacist or doctor if you have concerns.
What are safer alternatives to anticholinergic medications?
Depending on your condition, alternatives may include selective serotonin reuptake inhibitors (SSRIs) for depression or newer antihistamines for allergies. Non-drug therapies like cognitive behavioral therapy or lifestyle changes may also be effective.
Can lifestyle changes help reduce the need for medications linked to dementia?
Yes, in many cases, lifestyle modifications can alleviate symptoms that medications aim to treat. For example, dietary changes, increased physical activity, and stress management techniques can improve conditions like hypertension, anxiety, and insomnia, potentially reducing the need for certain medications.
How can I reduce my risk of dementia related to medication use?
Regularly review your medications with your healthcare provider, use the lowest effective doses, and explore non-pharmacological treatments when possible. Maintaining a healthy lifestyle with proper diet, exercise, and mental stimulation also supports cognitive health.
Are there screening tools to assess the risk of dementia related to medication use?
Healthcare providers can use tools like the Anticholinergic Risk Scale (ARS) to evaluate the cumulative anticholinergic burden of a patient’s medications. This assessment helps in making informed decisions about adjusting or discontinuing certain drugs to minimize dementia risk.
Quickly check Potency Level on this CRIDECO Anticholinergic Load Scale
Just enter the name of drug you are using and see what potency level it is and what it is used for.
Anticholinergic Risk Scale (ARS) Calculator Tool
This article is intended for informational purposes and should not replace professional medical advice. Always consult a healthcare professional before making changes to your medication or treatment plan.







