How Lyme Disease Affects the Brain
Did you ever wonder how Lyme disease impacts the brain, with symptoms like brain fog?
The U.S. Centers for Prevention and Control of disease estimates that approximately 200,000 people are diagnosed each year with Lyme disease.
But many believe the actual number of individuals experiencing Lyme in the Country is significantly higher.
That is because Lyme disease symptoms vary significantly and can impact people who are different in different ways.
Apart from that, the ELISA screening check most doctors use misses as much as thirty-five % of Lyme cases, making it a horrible first-line detection for the disease. (Screening assessments should have accuracy with a minimum of ninety-five percent.)
The issue is likely just going to deteriorate; being Lyme is of all the significant health consequences of climate change.
Despite many instances skipped in the doctor’s office, Lyme disease is also the most common tick-borne illness within the northern hemisphere.
Despite being so frequent, Lyme disease conditions differ based on the patient and how the bacteria impact various body methods.
Lyme disease often mimics some other health problems or conditions and be described as the brand new “great imitator.”
Lyme disease is frequently misdiagnosed as such illnesses, including:
- Chronic fatigue syndrome
- Fibromyalgia
- Multiple Sclerosis
- Dementia
- Alzheimer’s disease
- Autism-like syndromes
- Various psychiatric illnesses (For instance, a tick-borne infection may cause panic attack symptoms)
In approximately 15 % of cases, Lyme disease has a noticeable effect on the central nervous system. (That number may be more significant since public health officials recognize.
However, there are likely a substantial amount of predicaments of undiagnosed Lyme disease every year.)
Even with the noted powerful effects of theirs on the central nervous system, you can find numerous questions and unknown answers about what is going on during and working with the transmission of Lyme disease.
Let’s check Lyme disease and the central nervous system connection…
How Lyme Gets Into Your Brain
To know how Lyme Disease Affects the Brain, it is crucial to recognize the various phases of infection. (And exactly how the condition is transmitted in general.)
Ticks, specifically deer ticks in the northeastern U.S., would be the carriers of the germs spirochete Borrelia burgdorferi, which causes Lyme disease.
Mainly, the tiny, immature tick nymphs feast upon animals just like the white-footed mouse, squirrels, and other small mammals, which function as reservoirs for Borrelia burgdorferi.
Afterward, an infected tick is going to attach itself to another mammal or a person. When connected, the Tick is going to gorge on the blood of the host of its for a few days.
Infection Phase
Even before entering the body, S. Borrelia Burgdorferi has the work of its to do. Host blood goes into the tick gut during feeding, as S. Borrelia Burgdorferi instantly starts to multiply in planning to go on the tick’s salivary glands.
As the germs get into the body, several mechanisms make it hard for the immune system to strike and eradicate S. Borrelia Burgdorferi.
First, to avoid an immune response from the host body, the germs diminish the number of floor proteins, which signal a proinflammatory effect.
These proteins are generally found at high levels within the tick gut but are substantially reduced during feeding periods.
Additionally, there’s an upregulation of an additional surface protein that binds with inhibitor protein preserving the bacteria from the host immune system.
This particular protein’s increased expression is crucial for the survival of the disease within the host for the first forty-eight hours.
The germs likewise cause the expansion of anti-inflammatory cytokines, which play in modulating the body’s immune response. Scientific studies indicate that another way the Borrelia burgdorferi stay away from immune detection is by concealing.
The extracellular matrix of cells is considered immune-privileged and also, as it turns out, a great spot to hide. Borrelia burgdorferi can trigger a cascade of events that lead to the area expansion of a protein that digests the surrounding extracellular matrix.
This provides for the bacteria to connect to the matrix. Following the initial intrusion into the host, scientists think the bacteria use the bloodstream to increase permission to access other organs within the entire body, like the human brain.
How Lyme Disease Affects the Brain. Though it’s still unknown how the germs transverse the blood-brain barrier to access the brain, it’s believed the germs gain entry by’ slipping’ from the endothelial cells, which form the blood-brain barrier and by way of a transcellular passage.
After the bacteria is in the central nervous system, the regional body’s immune system will become activated. The immune cells that comprise dendritic cells, macrophages, and monocytes trigger the human brain’s proinflammatory result.
There’s a rise in chemokines, which, in turn, entice much more immune cells, causing an even much more massive inflammatory response.
How Lyme Disease Affects the Brain
How Lyme Disease Affects the Brain, Signs of the disease may start within days of a tick bite. Three great stages characterize symptoms: original localized, first disseminated, along with late given. The latter can affect the immune, neurological and cardiac systems.
The first localized stage occurs within weeks or days of the coming of the original infection. Occasionally, an erythema migrans rash, usually shaped like a bull’s eye, surfaces.
Although the Bull’s eye rash is regarded as a traditional sign of Lyme, it is present in just approximately fifty % of cases.
But Lyme rashes are not always Bull’s eyes. Research reveals several clinicians misdiagnose a Lyme related inflammation as spider bites, cellulitis, and shingles.
Days to days after disease, the germs disperse throughout the body in the early disseminated stage. These symptoms include:
- Fatigue
- Chills
- Fever
- Headache
- Stiff neck
Some or perhaps most of these signs might keep going for weeks, although intermittent, as well as fluctuate in intensity.
During this stage, individuals may start to display Lyme disease central nervous system symptoms, or perhaps intense Lyme neuroborreliosis, within many days to weeks of the original coming of the tick bite.
Lastly, when left unattended, Lyme disease progresses to a late disseminated stage a couple of months to years after the initial infection.
This particular phase’s symptoms include joint discomfort, arthritis, and a transition from intense neuroborreliosis to persistent neuroborreliosis.
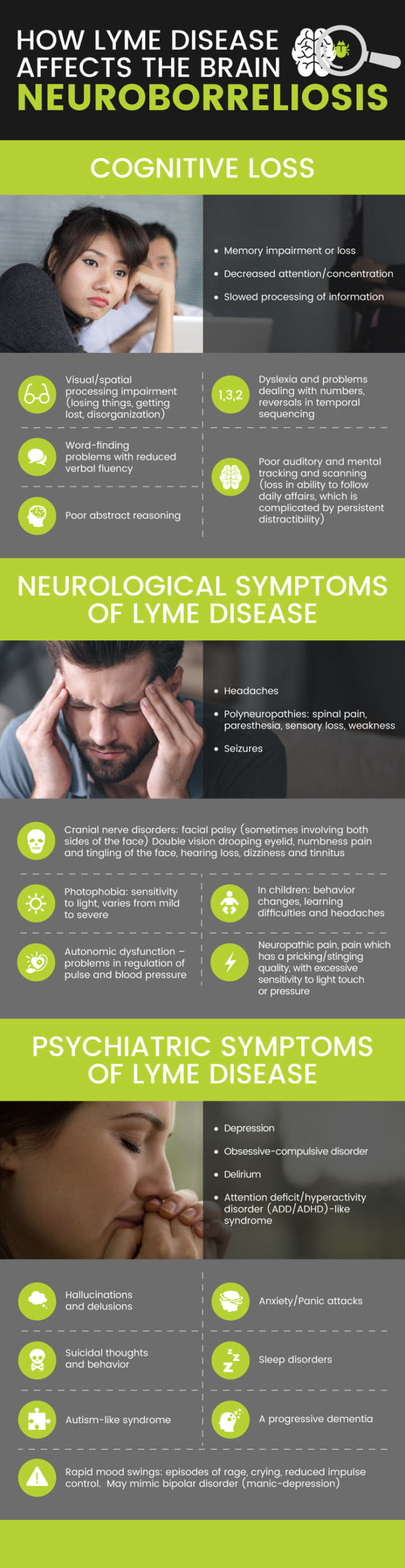
How Lyme Disease Affects the Brain: Neuroborreliosis
Among the most devastating areas of Lyme disease is neuroborreliosis. Patients often describe the quality of their life living with neuroborreliosis as being substandard.
The signs of neurological dysfunction are tremendous and can undoubtedly be classified into three categories:
Cognitive Loss
- Memory impairment or even loss
- Decreased attention/concentration
- Slowed processing of information
- Visual/spatial processing impairment (losing items, getting lost, disorganization)
- Dyslexia and difficulties coping with numbers, reversals in temporal sequencing
- Word-finding issues with decreased verbal fluency
- Poor abstract reasoning
- Mental tracking and low auditory and scanning (loss failure to stay with daily affairs, that is complex by chronic distractibility)
Neurological Symptoms of Lyme Disease
- Headaches
- Polyneuropathies: spinal discomfort, sensory loss, paresthesia, weakness
- Cranial nerve disorders: skin palsy (sometimes affecting each side of the experience), double vision, drooping eyelid, numbness, discomfort and tingling of the facial skin, hearing damage, tinnitus, and dizziness
- Neuropathic pain, pain that has a pricking/stinging quality, with too much sensitivity to light pressure or even touch
- Seizures
- Photophobia: awareness to lightweight, varies from mild to severe
- Autonomic dysfunction – issues in the regulation of heartbeat and blood pressure
- Mimic other defined neurological problems like Parkinson’s illness symptoms, M.S., Bell’s palsy, stroke, along with ALS, Encephalomyelitis
- In kids, indications of neurological participation may include headaches, learning difficulties, and behavior changes.
Psychiatric Symptoms of Lyme Disease
- Hallucinations as well as delusions
- Rapid mood swings: episodes of rage, crying, decreased impulse control. Could mimic bipolar disorder (manic-depression)
- Depression
- Suicidal behavior and thoughts
- Anxiety/Panic attacks
- Obsessive-compulsive disorder (OCD)
- Sleep disorders
- Attention-deficit/hyperactivity disorder (ADD/ADHD) like syndrome
- Autism-like syndrome
- Delirium
- A progressive dementia
The demonstration of neurological dysfunction brought on by S. Borrelia burgdorferi varies.
And although the pathophysiology behind it is still unclear, the principle is this: Scientists believe it is attributable to immediate cytotoxicity, neurotoxic (causing harm to neural cells/tissue) mediators, and triggered autoimmune reactions.
Cytotoxicity is the capability of cells to become poisonous and cause the demise of another section.
Within the human brain, astrocytes are cells that provide support for cells that make up the blood-brain barrier and help keep the nutrient source to neural tissue. S. Borrelia burgdorferi is found to induce astrogliosis, a practice of rapid cellular multiplication, and after that, cell death in astrocytes.
Borrelia burgdorferi has been proven to induce microglia and astrocytes to create poisonous substances, which may harm nerve cells, resulting in memory impairment, decreased focus, and exhaustion.
Like a decrease in tryptophan (a precursor to serotonin), alterations in neurotransmitter amounts may be involved in the psychiatric symptoms.
Varying neurotransmitter amounts might be to blame for the signs of tension, nervousness, and sleep disorders too. Finally, the induction of cytokines created by S. Borrelia burgdorferi is thought to cause an autoimmune-mediated reaction, which isn’t clearly understood.
How Lyme Disease Affects the Brain: Diagnosis Issues
There’s simply no independent reliable diagnostic test obtainable for Lyme disease because most testing we have resulted in false negatives or false positives.
Western blot and blood testing analysis can be worn but are not extremely sensitive, and the benefits may be inaccurate.
Individuals with persistent neurological symptoms could have late-stage Lyme and brain MRI disease testing done, which includes cerebrospinal fluid tests, in conjunction with various other testings to identify the existence of S. Borrelia burgdorferi.
Lyme disease head MRI scans might likewise show brain involvement. Interestingly, Lyme disease mind lesions sometimes appear on brain scans and seem much like multiple sclerosis lesions. Lyme condition lesions on the backbone are also possible.
The clinical representation of Lyme disease is usually a better method for diagnosis. Rashes are generally present, but not in most cases, and maybe very easily overlooked. The very best diagnostic option may be to use a few methods together since this condition has such prolific access to signs.
Treatment
Does Lyme’s head fog go out? I’ve seen folks with neurological Lyme disease signs feel very well again. And there are natural techniques to deal with Lyme disease.
In the opinion of mine, the actual because of chronic Lyme disease has damaged immunity, inhibited cellular function, and green factors. So to heal from Lyme disease, there is a great deal to address.
An individualized, integrative strategy might prove to function as the ideal treatment approach since there are many phases of the illness and far-reaching symptoms that affect several devices within the body.
Conventional therapy consists of oral antibiotics, even at times intravenous antibiotics. But there are additional supplemental treatments, hormonal therapies, immune modulators, including antivirals and food supplements.
A diet of anti-inflammatory food items like leafy green veggies, nuts, fish, and fruits may also help lower the disease’s autoimmune consequences.
Lyme disease head fog remedy, along with a neurological Lyme disease remedy, will probably call for a suite of lifestyle modifications and the best supplements for the specific situation of yours, incorporating a focus on repairing methylation problems.
Prevention
Many preventive measures could be considered to lessen the danger of contracting Lyme disease.
- First, before outdoor activities, use a homemade bug spray to repel ticks.
- Other non-toxic tick repellents are essentials oils like lavender, lemongrass, peppermint, tea tree, rosemary, and sage. Lemongrass possesses tick repelling properties.
- When hiking outdoors or perhaps playing in higher or wooded lawn areas, use long sleeves and long pants tucked into socks or perhaps cuffed at the bottom part.
- Wear light-colored clothing so that you can spot ticks easier and eliminate them immediately.
- Following outside activities, change clothing promptly and put them within the washer/dryer.
- Look for ticks immediately; because the nymphs are tiny and are usually overlooked, search for a rash a couple of days following the event.
Final Thoughts on How Lyme Disease Affects the Brain
- Lyme disease is prevalent in the U.S., and lots of people have the illness and do not realize it.
- Symptoms vary and affect almost every system of the entire body.
- Since characteristic symptoms are extensive ranging and diffuse, it’s often hard to diagnose this disease.
- There’s no single right diagnostic method.
- How does Lyme disease impact the human brain? Neuroborreliosis affects a person’s neurological and cognitive functions and causes different psychiatric problems that severely minimize an individuals’ quality of living.
- Far more study should be done to understand neuroborreliosis better so that a proper analysis testing product may be used.