How to Cure Herpes Permanently
HERPES is among the most frequent sexually transmitted diseases (S.T.D.s), prompting most of us to question how we can eliminate herpes naturally and it can be done at all?.
The virus can stay dormant inside a person’s body’s immune system for a lifetime, occasionally causing blisters that burst and become open cold sores or perhaps ulcers before healing.
On your own, herpes cold sores typically last approximately 10 to 14 days and therefore are uncomfortable for various reasons – often causing burning, pain, and redness along with embarrassment.
DEFINITION
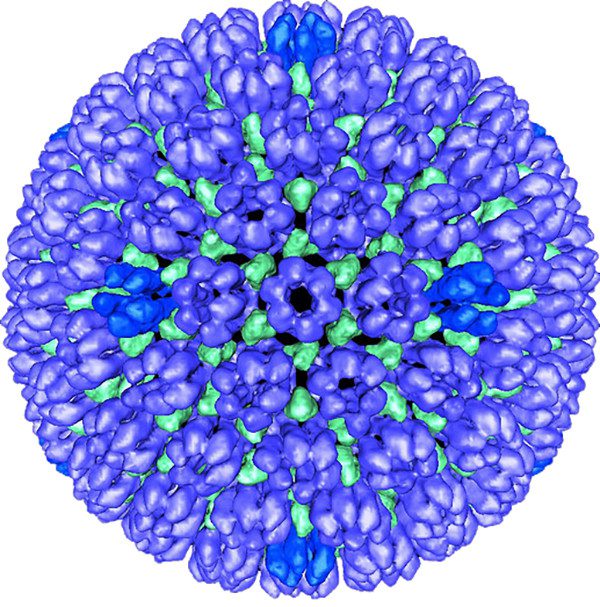
Herpesviruses fall within the family Herpesviridae. This family includes the herpes simplex viruses: herpes simplex virus type 1 (HSV-1) and herpes simplex virus type 2 (HSV-2).
These two viruses cause blister-like open sores, usually on the mouth (HSV-1) or genitals (HSV-2) of the infected person.
DESCRIPTION
HSV-2, or genital herpes, is a sexually transmitted disease (STD) and usually is associated with genital ulcers or sores.
HSV-1, which is transmitted from person to person by close contact such as kissing or sharing eating utensils, usually is associated with infections of the lips, mouth, and face; its sores are associated to as “oral herpes,” “cold sores,” or “fever blisters.”
HSV-1 may also cause genital herpes, but HSV-2 is the leading cause of genital herpes. Other herpes viruses that infect humans include:
- Human herpesvirus 3 (HHV-3), also known as herpes zoster virus or varicella-zoster virus, is the cause of chickenpox. This virus lies dormant in the body. In some cases, it may re-activate later in life, causing shingles (herpes zoster), which results in a painful rash and, in some cases, continuing nerve pain (postherpetic neuralgia), temporary partial facial paralysis, or other problems.
- Human herpesvirus 4 (HHV-4), also known as the “Epstein-Barr virus,” causes infectious mononucleosis, or “mono” (sometimes known as “the kissing disease”). It is also associated with Hodgkin lymphoma and specific other cancers.
- Human herpesvirus 5 (HHV-5) is also known as “cytomegalovirus.” Most people have no symptoms from this virus, but congenital disabilities can occur in infants born to women who have primary (first) infections with cytomegalovirus during pregnancy. Besides, individuals who are immunocompromised can develop an infection-related illness.
- Human herpesvirus 6 (HHV-6) is a set of two viruses, HHV-6A and HHV-6B. Infection with HHV-6B can cause roseola (exanthem subitum rash) and fever, and diarrhea in infants. Although rare, some infants experience seizures and encephalitis. If re-activated later in life, the virus can cause symptoms, which occasionally include the brain’s infection, leading to cognitive dysfunction and even death.
- Human 6herpesvirus 7 (HHV-7) is similar to HHV-6, although it causes roseola less frequently.
- Human herpesvirus 8 (HHV-8), also known as “Kaposi’s sarcoma-associated herpesvirus (KSHV),” because it causes Kaposi’s sarcoma, a sort of cancer that commonly occurs in patients who have acquired immunodeficiency syndrome (AIDS).
DEMOGRAPHICS
Herpes viruses are prevalent worldwide. As of 2010 in the United States, 16.2% of people aged 14–49 years had genital HSV-2 infection, corresponding to the Centers for Disease Control and Prevention.
The virus moves from an infected male to a female partner more quickly than from an infected female to a male partner.
It is, therefore, more common among women (about 20% of the population aged 14–49) than among men (about 11% of the population aged 14–49).
As of 2010, the prevalence was higher among African Americans, with 39.2% of the population experiencing HSV-2. Among African American women, the majority of HSV-2 is 48%.
Exposure to other herpes viruses is even more common. Estimates of the infection rate for HSV-1 are as high as 90%. HHV-6 is similarly a nearly universal infection.
It is responsible for up to 20% of all fever-associated infant visits to U.S. emergency rooms.
Between 50% and 80% of adults in the United States have had a CMV infection by age 40.
About 90% of all Americans have been exposed to the chickenpox virus by the time they are 15 years old.
Those who have had the chickenpox vaccine may have no or only mild symptoms.
CAUSES AND SYMPTOMS
Causes
The herpes viruses are spread in many ways. HSV-1 is transmitted by close contact, including kissing.
HSV-2 is sexually transmitted, and risk factors for HSV-2 infection include having many sexual partners and unprotected sex.
HSV-2 can also be spread by oral sex and cause sores on the lips.
People acquire HHV-3, chickenpox virus, infections through direct contact with broken chickenpox blisters on an infected individual, contact with a recently contaminated item (such as a ball that an infected person was handling), and through airborne droplets expelled via coughing or sneezing.
Some herpesviruses may also be transmitted from a mother to her unborn child.
Symptoms
Symptoms vary among the different types of herpes. HSV-1 and HSV-2 cause sores on mucous membranes, most often in the mouth and the genital region.
Once HSV-1 and HSV-2 enter the body, they spread to nearby mucosal areas through nerve cells.
Typically, 50–80% of people with oral herpes encounter a prodrome (symptoms of oncoming disease) of pain, burning, itching, or tingling at the place where blisters will develop.
This prodrome stage may last anywhere from a few hours to one or two days. The herpes infection prodrome occurs in both the primary infection and recurrent infections.
When one of the sexually transmitted Herpes Virus 2 cells goes into the entire body through genital cells, it travels to neurons near the spinal column. The body’s defenses have instructions not to kill – even when infected – since these cells do not regenerate quickly.
Moreover, the disease hides, often reactivating blisters, which can break to bring about painful sores.
Ready to invade a next sexual partner.
“Once your neurons get afflicted, you can never eliminate the infection,” stated Dr. Akiko Iwasaki, a Howard Hughes Medical Institute Investigator.
“But in case we can inhibit replication of the disease, we can make the result milder and help folks suffering from this particular ailment.”
Though We Can not Cure Herpes Permanently
The W.H.O. estimates that 536 million people between the ages of fifteen and forty-nine worldwide live with Herpes Virus -2 (HSV 2) or approximately sixteen % of the world’s public within that particular age span.
HSV-2 affects females more than males, leaving them susceptible to transport the condition to their newborn kids, which is usually fatal.
Additionally, HSV 2 dramatically increases the chance of disease by H.I.V., the virus which causes AIDS.
Ever since receiving the very first of 2 seed grants from Female’s Health Research at Yale in 2003, Iwasaki’s laboratory has gained more significant financing mainly from the National Institutes of Health for scientific studies, which have determined groundbreaking insights into the transmission, potential prevention, and treatment of Herpes Virus.
“Women’s Health Research at Yale has helped us stand up and run,” Iwasaki said. “Fifteen years back, practically nothing was known about the immune safeguard of genital cells. So now we are getting to crack the puzzle.”
The obstacles to creating a suitable vaccine that protects somebody from contracting herpes involve the disease itself and the tissue just where it usually enters the body.
Most vaccines generate antibodies – the body’s organic defenses that attack invading microorganisms, resulting in disease.
However, viruses as H.I.V., as well as influenza mutate to escape detection, as well as HSV, have coat proteins that permit them to get away antibody clearance. This will make an antibody-based universal vaccine very hard to develop.
Instead, Dr. Iwasaki’s staff has attempted to marshal infection-fighting cells called T lymphocytes, which realize stretches of the virus’ natural protein-rich foods that are much less prone to mutate without affecting the vital functions theirs.
“We are trying to create a shield with T cells that the virus cannot escape,” Iwasaki said.
Nevertheless, T cells do not survey vaginal tissue in high numbers, prompting Iwasaki’s staff to make a brand new vaccine technique they call the “prime & pull” method.
This involves primarily stimulating the body to create a memory response to HSV 2 then drawing the T cells to the vagina with the immediate application of small protein-rich signaling molecules known as chemokines.
Female’s Health Research at Yale has helped us to stand up and to run. Fifteen years back, virtually nothing was known about the immune safeguard of genital cells. So now we are getting to crack the puzzle.
Symptoms of the primary infection of HSV-1 and HAV-2 usually are more severe than those of recurrent infections.
The primary infection can cause symptoms similar to those shown in other viral infections, including shortness of power, headache, fever, and swollen lymph nodes in the neck.
The first sign of infection is the formation of fluid-filled blisters that may last up to two weeks. However, the pain in the area may last much longer.
Once an individual becomes infected with HSV-1 or HSV-2, the virus remains in the body for that individual’s life. (This is true of other herpes viruses, too.)
During periods of latency, the patient has no symptoms. At times, the infected person may shed the virus into their saliva and genital secretions and infect others.
Peeling can happen even in the absence of visible symptoms. Individuals infected with the virus can have recurrent infections or flare-ups; however, recurrent infections usually have milder and shorter symptoms.
Nevertheless, cancer patients and others with compromised immune systems can have severe recurrences and serious complications.
Women who develop a primary HSV-2 infection during pregnancy are at greater risk of delivering babies with congenital disabilities.
Active genital herpes sore at the time of birth can cause severe results for the baby. These include blindness, congenital disabilities, and even death in the baby.
Cesarean section may be advisable for mothers with active herpes sores at the time of delivery.
DIAGNOSIS
Often, infection with HSV-1 or HSV-2 is diagnosed from the patient’s description of symptoms and visual examination of the sores.
If uncertainty remains about a sore’s culprit, a tissue specimen or culture may be extracted to check what type of virus or other microorganism is responsible.
For herpes, it is preferable to have this test done within the first 48 hours after symptoms first appear for a more accurate result.
Testing for neonatal HSV infections may include:
- Unique smears and/or viral cultures.
- Blood antibody levels.
- Polymerase chain reaction (PCR) testing of spinal fluid.
Cultures are usually obtained from skin vesicles, eyes, mouth, rectum, urine, stool, and blood.
TREATMENT
There is no cure for HSV infection.
Usually, the sores clear without treatment. It is essential to keep the blisters or sores clean and dry with an agent such as cornstarch until they do.
One should avoid touching the sores and wash hands frequently. Local application of ice may relieve the pain.
Over-the-counter medication for fever, pain, and inflammation, such as aspirin, acetaminophen, or ibuprofen, may help.
Kids should never be administered an aspirin because of the possible development of Reye’s syndrome.
During an outbreak of HSV cold sores, the patient should avoid salty foods, citrus foods (e.g., oranges), and other foods that irritate the sores.
Over-the-counter lip medicaments that contain the chemical “phenol” (such as many medicated lip ointments) and numbing agents (such as the ointment Anbesol) help to relieve the pain of cold sores.
A bandage can be arranged over the sores to protect them and to stop spreading the virus to other places on the lips or face.
Sexual intercourse should be avoided during both the HSV active and prodrome stages.
Drugs
Antiviral drugs have some effect in lessening HSV infection symptoms, decreasing the length of herpes outbreaks, and preventing immunocompromised individuals’ complications.
For the best results, drug treatment should begin during the prodrome stage before blisters are visible.
Depending upon the length of the outbreak, drug treatment could continue up to 10 days. Antiviral medications include acyclovir (Zovirax), famciclovir (Famvir), and valacyclovir (Valtrex).
All are administered in pill form. For severe cases, acyclovir may also be administered intravenously.
Acyclovir, a commonly prescribed medication, effectively treats both the primary infection and recurrent outbreaks and can reduce the frequency of herpes outbreaks.
PROGNOSIS
Infection with HSV is permanent. Although symptom-free periods are standard, individuals may still shed the virus and infect others during these times.
Life-threatening neurological complications may occur in immunocompromised individuals, and HSV-2 infection during pregnancy and delivery can cause congenital disabilities or severe harm to the infant.
PREVENTION
It is almost impossible to prevent HSV-1 infection. Restricting the number of sex partners reduces the likelihood of contracting HSV-2.
Using a condom may help discourage disease but does not fully protect against the spread of the virus.
EFFECTS ON PUBLIC HEALTH
Genital herpes, in particular, is a public health concern because it is one of the most prevailing sexually transmitted illnesses in the United States.
Many people who have the disease fail to recognize that their symptoms are related to genital herpes.
Therefore, they continue their normal sexual behavior, which can transmit it to their partners.
Even those who have the disease and are vigilant about avoiding sexual relations while they have outbreaks may spread the virus to their partners.
Genital herpes is widespread in some populations (almost 40% of African Americans overall and nearly 50% of African American women are infected with HSV-2).
Such a high incidence of this disease hampers its containment.
COSTS TO SOCIETY
The United States’ annual direct medical costs for genital herpes have been estimated as high as $984 million, with nearly half going to drug expenditures and another 48% to outpatient medical care.
Lost productivity due mainly to days off for sickness or time spent for treatment accounted for a further $214 million.
A single case of neonatal herpes was estimated to result in $60,000 in medical costs.
EFFORTS AND SOLUTIONS
A vaccine for HSV-1, and especially for HSV-2, would help to stem the incidence of genital herpes.
Work on that front is continuing. Hopes were high for an investigational HSV-2 vaccine.
Still, a research article in a 2012 edition of the New England Journal of Medicine found that while the vaccine effectively prevented HSV-1, it was ineffective against HSV-2, which causes most genital herpes.
A study that appeared in a 2012 issue of The Lancet demonstrated that the frequency of HSV-2 shedding was reduced in individuals who used acyclovir compared to those who used no medication.
It also showed an advantage for high doses of antiviral drugs: High-dose acyclovir and high-dose valaciclovir each resulted in less frequent shedding than standard doses of the medications.
Nonetheless, shedding occurred even with high doses of the drugs, and transmission of the virus between sexual partners still occurred, although at a lower rate.
The authors concluded, “Short bursts of subclinical genital HSV re-activation are recurrent, even amid high-dose antiherpes therapy, and possibly account for the continued spreading of HSV during suppressive antiviral medication.
Stronger antiviral therapy is needed to eliminate HSV transmission.”
Another intriguing avenue of research involves Alzheimer’s disease, which affects about 20 million people worldwide.
Researchers have uncovered a potential link between HSV-1 infection and an increased risk for Alzheimer’s disease, especially in individuals with a specific genetic factor.
Additional studies on the possible connection are underway.
One study, published in 2011 by researchers in the United Kingdom, considered the possibility that antiviral agents against HSV1 might slow the progression of Alzheimer’s disease and found evidence that it might do just that.
Their findings suggested that the antiviral agents significantly reduced the levels of proteins associated with Alzheimer’s disease and could be a potential treatment vector.
Resources
Baker, Carol J., ed. Red Book Atlas of Pediatric Infectious Diseases, 4th ed. Itasca, IL: American Academy of Pediatrics, 2019.
Cristaudo, Antonio, and Massimo Giuliani, eds. Sexually Transmitted Infections: Advances in Understanding and Management. New York: Springer, 2019.
Diefenbach, Russell, and Cornel Fraefel, eds. Herpes Simplex Virus: Methods and Protocols, 2nd ed. Totowa, NJ: Humana, 2019.
Forbes, Harriet, et al. “Risk Factors for Herpes Simplex Virus Type-1 Infection and Reactivation: Cross-Sectional Studies among EPIC-Norfolk Participants.” PLoS ONE 14, no. 5 (2019): e0215553.
Ma, Wenqing, et al. “Oncolytic Herpes Simplex Virus and Immunotherapy.” BMC Immunology 19, no. 1 (2018).
Shrivastava, Saurabh, et al. “Rising Trends of Herpes Simplex Virus – 1: A Global Public Health Concern.” Indian Journal of Sexually Transmitted Diseases and AIDS 40, no. 1 (2019): 77.
“Genital Herpes.” Centers for Disease Control and Prevention. January 4, 2017. https://www.cdc.gov/std/Herpes/default.htm (accessed June 10, 2019).
“Genital Herpes.” Mayo Clinic. October 3, 2017. https://www.mayoclinic.org/diseases-conditions/genital-herpes/symptoms-causes/syc-20356161 (accessed June 10, 2019).
“Herpes Simplex.” MedlinePlus. November 2, 2018. https://medlineplus.gov/herpessimplex.html (accessed June 10, 2019).
“Shingles.” Mayo Clinic. May 16, 2018. https://www.mayoclinic.org/diseases-conditions/shingles/symptoms-causes/syc-20353054 (accessed June 10, 2019).
“Shingles (Herpes Zoster).” Centers for Disease Control and Prevention. October 17, 2017. https://www.cdc.gov/shingles/index.html (accessed June 10, 2019).
American Social Health Association, P.O. Box 13827, Research Triangle Park, NC 27709, (919) 361-8400, (800) 227-8922, (919) 361-8425 http://www.ashastd.org.
Centers for Disease Control and Prevention (CDC), 1600 Clifton Rd., Atlanta, GA 30333, (800) 232-4636 cdcinfo@cdc.gov, http://www.cdc.gov .
National Institute of Allergy and Infectious Diseases (NIAID), 6610 Rockledge Dr., MSC 6612, Bethesda, MD 20892, (866) 284-4107 http://www.niaid.nih.gov/Pages/default.aspx.
Belinda M. Rowland, PhD
Revised by Tish Davidson, AM Leslie Mertz, PhD