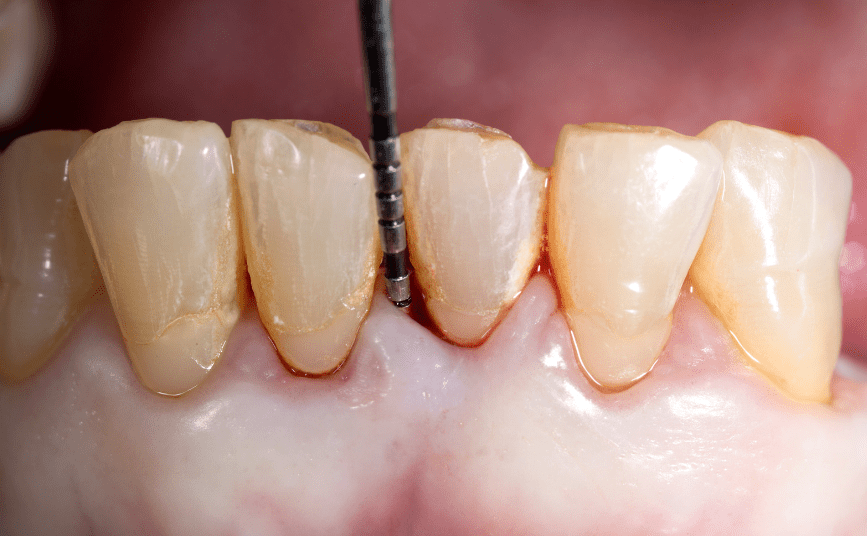
Oral hygiene instructions and non-surgical periodontal tissue regeneration treatment comprise the initial periodontal treatment aiming to reduce plaque accumulation, calculus deposits, gingival inflammation, and pocket depths.
It is also effective for gaining attachment levels. However, non-surgical periodontal treatment rarely translates into periodontal regeneration. In patients with severe periodontal disease, residual periodontal pockets may remain after initial therapy.
These residual periodontal pockets can be eliminated at the second phase of the treatment by resective (osseous surgery, modified Widman flap, apically positioned flap) or regenerative procedures based upon the morphology of the defect.
Regeneration of the periodontal tissues includes cementum, periodontal ligament (PDL), and alveolar bone.
Several flap designs and biomaterials have been utilized and tested in the literature aiming at periodontal regeneration, including bone grafts, bone substitute materials, growth factors, enamel matrix derivative proteins (EMD), guided tissue regeneration, or even a combination of these materials.
Periodontal disease is a multifactorial inflammatory disease that destroys the supporting tissues around teeth, including periodontal ligament, cementum, and alveolar bone.
Among all the causes of tooth loss, it is the most common if left untreated. It is important to emphasize that non-surgical periodontal treatment rarely translates into periodontal regeneration.
In patients with severe periodontal disease, residual periodontal pockets may remain after initial therapy.
Elimination of residual periodontal pockets after non-surgical periodontal therapy can be achieved either with resective treatment (osseous surgery, apically positioned flap, modified Widman flap) or by regenerative procedures.
Periodontal Tissue Regeneration Treatment
Regeneration of the periodontal tissues includes new cementum, new periodontal ligament, and new alveolar bone.
Barrier membranes for guided tissue and guided bone regeneration need to exhibit specific characteristics, including biocompatibility, proper degradation profile, good mechanical and physical properties, and sufficient sustained strength targeting avoidance of membrane collapse.
Absorbable and non-absorbable membranes have been tested in the literature, while the significant advantage of absorbable membranes is the need for only a single surgery.
Membrane surface topography, chemical composition, and porosity may have an effect on cell proliferation, including PDL cells.
According to a review published by Cortellini and Tonetti, using absorbable collagen membranes in periodontal regenerative treatment is an effective and predictable treatment modality.
Non-absorbable membranes are associated with an increased risk of membrane exposure, approximately 70-80%, with a high risk for contamination. However, a flap design that preserves the papillae can reduce such a risk.
Periodontal Regenerative Treatments
Several factors have been highlighted for their significant effect on the clinical outcomes in periodontal regenerative treatments. Smoking has been significantly associated with poor wound healing and reduced treatment outcomes, as has as poor oral hygiene.
The defect size is another critical parameter. Narrow and deep defects that are well-contained with at least 3 mm of depth have led to more predictable attachment level gain and bone fill compared to non-well-contained defects of <3 mm depth.
The defect angle also plays a crucial role in periodontal regenerative procedures.
Radiographic defect angle of <25 degrees consistently shows more excellent attachment gain than those with > 25-degree angle. Finally, tissue thickness, circumference defect, and the number of bony walls play an important role.
More specifically, tissue thickness of >1 mm, absence of circumference defects, and presence of intact bony walls result in higher predictability and more significant attachment gain and bone fill.
Periodontal regeneration in two- or three-wall defects is more predictable than in one-wall defects.
The increased gingival recession following periodontal regenerative procedure with GTR, as well as the high membrane exposure rate, has led several investigators to test different flap designs.
Flap Design
In periodontal plastic surgery procedures, the flap design and the control of various risk factors play a critical role in the treatment outcome.
The flap design is based on the vascularization of the periodontal tissues. It is essential to highlight the importance of sulcular incisions compared to marginal or paramarginal incisions, avoiding vertical incisions, and periosteal-releasing incisions when possible.
Today, conservative flap designs have been suggested utilizing minimal flap reflection that would lead to retention of primary closure and less gingival recession.
Primary closure of the flaps is also of significant value. Vertical incisions release the flap, measured at approximately 1 mm when only one vertical incision is performed and 2 mm when two are made. Alternatively, soft tissue graft can predictably lead to primary closure.
In a study with an absorbable collagen membrane, simplified papilla preservation was performed, leading to ~30% of membrane exposure between the second and sixth weeks post-surgery.
It also led to a significant attachment gain and pocket-depth reduction, reaching a 5 mm change. Gingival recession was also evident and was statistically significant compared to the baseline.
The use of papilla preservation with GTR was compared with papilla preservation alone in a multicenter study. GTR revealed a statistically significant greater CAL gain and PPD reduction than the access flap group.
Still, it is essential to mention that the first group had statistically significant more profound intrabony defects and higher PPD and CAL at baseline compared to the control group, which means that it was expected that more profound intrabony defects would have resulted in more significant attachment level gain and bone fill.
In another multi-center study, GTR with Bio-oss and papilla preservation yielded statistically significantly more significant radiographic bone fill, radiographic resolution of intrabony defect, PPD reduction, and CAL gain compared to papilla preservation alone.
In that study, patients with similar defect characteristics at baseline, primarily two-wall defects, were treated with either GTR plus Bio-oss or access flap only and were followed up for one year post-operatively.
The GTR treatment showed significantly more significantly improved hard and soft tissue response. At the same time, initial pocket depth and baseline gingival inflammation had an essential effect on the treatment outcome.
On the other hand, smoking, plaque control, and radiographic angle of the intrabony defect did not influence the outcome.
GTR With or Without Bone Graft Materials
The effect of GTR with or without bone graft material or combined with enamel matrix derivatives (EMD), platelet-derived growth factor (PDGF), and calcium sulfate has been tested in the literature.
GTR and treatment of intrabony defects with graft materials have shown superior clinical attachment level (CAL) gain and probing pocket depth (PPD) reduction compared to open flap debridement (OFD) alone. Still, the results vary among the several studies.
Bio-oss with GTR was compared with OFD in a human study of non-smokers with intrabony defects. Both groups consisted of mainly two-wall defects, and the baseline characteristics of the defects were similar.
Both treatment modalities showed significant reductions in pocket depth and significant attachment level gain one and five years after the surgery, while no differences were observed between the two groups.
It is also important to mention that both treatments led to significant gingival recessions after the treatment, which were insignificantly greater in the GTR-treated group compared to the OFD-treated group.
Comparison of Trials
GTR in combination with calcium sulfate was compared to GTR alone and OFD by Paolantonio et al. in a re-entry study of 12 months.
Intrabony defects with two or three walls and similar clinical characteristics at baseline were included in the study. Re-entry surgeries showed that all clinical parameters were improved for all treatment modalities at one year.
Still, GTR alone and GTR with calcium sulfate showed significantly less PPD and CAL than the OFD alone group. However, membrane exposure and calcium sulfate exposure were reported.
Regarding the periodontal regenerative treatment of furcation defects, non-absorbable membranes and collagen membranes with or without bone graft have been tested.
Mandibular molars were used in a study by Luepke et al. They were treated with GTR alone or a combination of GTR with demineralized freeze-dried bone allograft (DFDBA) and followed up for six months.
At that time, a re-entry surgery was performed. Both treatments led to statistically significant PPD reduction, CAL gain, and vertical and horizontal bone fill, but GTR with DFDBA showed superior clinical results compared to GTR alone.
Non-smokers responded better to treatment with GTR plus DFDBA, with more significant vertical bone fill, CAL gain, and PPD reduction.
In another study that compared ePTFE membrane and collagen membrane to treat furcation grade II defects in mandibular molars, no difference was observed among the groups.
In contrast, a significant improvement was observed, including furcation closure or change from grade II to grade I furcation involvement, in the vast majority of the included cases.
Both treatments led to adverse events such as suppuration and abscesses, with no significant differences in their frequencies.
In another study by Eickholz and colleagues, similar results were seen, with similar vertical and horizontal attachment level gain.
Bowers and coworkers attempted to identify potential factors related to the complete closure of the furcation defects after treatment with ePTFE membranes and DFBDA.
They found that initial probing depth, anatomical features of the furcation (root trunk, root divergence), the distance between the roof of the furcation to the base of osseous defects and the alveolar crest, as well as bone height in the interproximal area, are critical factors for the success of the treatment.
These findings were expected because it is critical for the grafting materials to have a blood supply. The ability to clean the root surfaces to have biologically compatible ones plays a significant role.
Treatment of furcation defects with autogenous bone has shown an increased risk for root resorption, while root conditioning does not generally improve clinical results.
Enamel Matrix Derivative (EMD)
EMD plays a significant role in mediating cell attachment, spreading, proliferation, differentiation, survival, and expression of transcription factors, growth factors, cytokines, extracellular matrix constituents, and other molecules that regulate bone remodeling.
It has also been found that EMD influences wound healing, favoring soft tissue regeneration and angiogenic activity.
EMD has been tested in two randomized clinical trials as an adjunct to non-surgical periodontal therapy showing no additional benefit. However, EMD can be effectively used in intrabony defects, furcation defects, and gingival recessions, improving soft tissue height and width.
Over 20 years, no patient allergic reactions or adverse events have been reported about using EMD.
Systematic reviews and meta-analyses have compared the effectiveness of various bone graft procedures and EMD for treating intrabony defects.
Two systematic reviews of randomized, controlled clinical trials on patients diagnosed with periodontitis having intrabony defects of at least 3 mm treated with EMD compared with OFD, GTR, and various bone graft procedures with at least one-year follow-up showed that the treatment with EMD exhibited a significant additional gain in CAL of 1.1-1.3 mm and PPD reduction of 0.9 mm compared to OFD.
GTR and EMD showed similar clinical improvement, while GTR displayed statistically significant more postoperative complications and recession. The use of EMD in furcations in one included study showed similar horizontal defect depth reduction compared with resorbable membranes.
EMD + coronally advanced flap demonstrated similar outcomes with connective tissue graft and significantly better outcomes than coronally advanced flap alone.
The clinical effectiveness of EMD alone or in combination with bone grafts and bone substitute materials was tested in several studies.
Lekovic and colleagues included 21 paired intrabony defects of >6 mm and were treated with either EMD alone or EMD combined with bovine porous bone mineral.
In that re-entry study that included two- and three-wall defects (equally distributed), the combination treatment showed a more significant reduction in buccal and lingual measurements, significantly higher gain in clinical attachment and more excellent defect fill than the EMD alone group.
The superiority of the combined treatment could be attributed to the osteoconductive and/or osteoinductive properties of the graft material or even to the space-making effect of the graft.
In a similar split-mouth study, 16 adult patients with moderate to severe chronic periodontal disease with at least two intrabony defects of PPD>=5 mm were treated with either EMD alone or EMD + bovine-derived xenograft.
Soft and hard tissue measurements, teeth location, and defects’ anatomical features were similar in both groups at baseline.
In contrast, the combined grafting group showed statistically significant higher bone fill (4 mm versus 3.1 mm) and less gingival recession (0.8 mm versus 0.3 mm) than EMD alone.
PPD reduction, CAL gain, crestal resorption, bone fill, and percentage of defect resolution did not present any statistically significant differences among the groups.
The use of EMD with or without bioactive glass has been tested in intrabony defects of non-smokers by Sculean and colleagues, showing statistically significant reductions in PPD, gains in CAL, and an increase in gingival recession four years following surgery when strict maintenance was applied.
Both treatments resulted in significant clinical improvements, but none showed any superiority over the other.
When EMD was compared with ePTFE membranes, absorbable membranes, and absorbable membranes + bone graft, no statistically significant differences were observed among groups.
Still, all of them led to significant clinical improvements. However, it is worth mentioning that EMD-treated defects were three-wall defects, while ePTFE membranes were one- and two-wall defects.
Growth and Differentiation Factors
Molecular and cellular advances have led to the development of several growth and differentiation factors that are biological mediators for the development and growth of tissues and organs.
Factors such as platelet-derived growth factor (PDGF), insulin-like growth factor I and II (IGF-I, -II), acidic and basic fibroblast growth factors (a,b FGF), transforming growth factor-beta (TGF-beta), and bone morphogenetic proteins (BMP) may also support wound healing and regeneration of periodontal tissues.
To date, the only commercially available growth and differentiation factors for periodontal indication would be PDGF-B, while BMP-2 and BMP-7 are available in maxillofacial and orthopedic surgery.
Delivery systems for growth factors may play a crucial role in the treatment outcome, including collagen as a sponge, membrane, gel, or gelatin.
Lynch et al. hypothesized that the combination of PDGF-B and IGF-I can enhance periodontal regeneration.
They endeavored to determine the length of time it must be present at the healing site to achieve its goal.
To test this hypothesis, they performed conventional periodontal surgery on all four quadrants of 12 beagle dogs with naturally occurring periodontal disease.
They demonstrated that the short-term application of this combination significantly enhanced the wound healing events, leading to a significant amount of new bone and cementum formation five weeks following surgery.
The application of rhPDGF-BB incorporated in bone allograft showed a robust regenerative response in interproximal intrabony defects and class II furcation defects with extensive bone formation, well-organized new PDL, and extensive new cementum.
Regarding the intrabony defects, the vertical pocket depth reduction was 6.4 mm, the clinical attachment level gain was 6.17 mm, and the radiographic bone fill was 2.14 mm.
Concerning the furcation defects, rhPDGF plus allograft showed a mean horizontal, and vertical pocket depth reduction of 3.40 mm and 4.00 mm, respectively, and the attachment gain was 3.2 mm.
In a study by King et al., rhBMP-2 stimulated cell recruitment following periodontal wound healing, leading to a more rapid healing response.
The rhBMP-2 induced the proliferation and migration of cells from the adjacent unwounded PDL into the wounded areas during the early stages of wound healing and promoted a nearly three-fold increase in new cementum formation, thus increasing the periodontal regeneration in Wistar rats.
Kwon and colleagues evaluated the effect of a novel rhGDF-5 construct intended for onlay and inlay indications on periodontal wound healing in five mongrel dogs with contralateral surgically created 6 mm supra-alveolar periodontal defects.
Sites that received rhGDF-5 + [beta]-TCP + PLGA showed 2.4 times greater bone formation, 2.1 times greater cementum formation, and insignificant increased PDL formation, bone area, and density compared to [beta]-TCP and PLGA-treated sites.
A similar incidence of root resorption was found among the groups, while an increased risk for ankyloses characterized the test group.
These results agree with a literature review article by Moore et al. that highlighted the increased bone formation, fracture healing, and cartilage and ligament formation after applying GDF-5. GDF-5 also enhances endosseous implant stability in trabecular bone, accelerating bone formation and integration in the maxillary sinus and in mandibular alveolar defects.
Kitamura and colleagues demonstrated the effectiveness and safety of FGF-2 in regenerating human periodontal tissues in intrabony defects. (30,31) FGF-2 demonstrated significant superiority over the vehicle alone regarding the percentage of bone fill, which reached a plateau in the 0.3% dose.
The rhFGF-2 showed a significantly more significant percentage of bone fill (37.1% versus 21.6%) compared to the placebo group, while no differences were observed in terms of CAL gain.
When rhFGF-2 was compared to EMD, at 36 weeks, the bone regeneration was 1.9 mm in the rhFGF-2 compared to 1.36 mm in the EMD, and the percentage of bone fill was more significant in the rhFGF-2 group than it was in the EMD group (37.1% vs. 21.6%).
These findings, in conjunction with the absence of clinical/safety problems in both studies, led the authors to conclude that it is an effective and safe treatment for periodontal regeneration in intrabony defects and superior to the treatment with EMD.
References
(1.) Offenbacher S. Periodontal diseases pathogenesis. Ann Periodontal 1996;1:821-878.
(2.) Bottino MC, Thomas V, Schmidt G, et al. Recent advances in developing GTR/GBR membranes for periodontal regeneration – A materials perspective. Dent Mater 2012;28:703-21.
(3.) Cortellini P, Tonetti MS. Focus on intrabony defects: guided tissue regeneration. Periodontology 2000 2000;22:104-132.
(4.) McClain PK, Schallhorn RG. The use of combined periodontal regenerative techniques. J Periodontol. 1999;70:102-4.
(5.) Burkhardt R, Lang NP Fundamental principles in periodontal plastic surgery and mucosal augmentation – a narrative review. J Clin Periodontol 2014;41 Suppl 15:S98-107.
(6.) Cortellini P, Prato GP. Tonetti MS. The simplified papilla preservation flap. A novel surgical approach for the management of soft tissues in regenerative procedures. Int J Perio Rest Dent 1999;19:589-599.
(7.) Tonetti MS, Cortellini P. Suvan JE et al. Generalizability ot the added benefits of guided tissue regeneration in treating deep intrabony defects. Evaluation in a multi-center randomized controlled clinical trial. J Periodontol 1998;69:1, 183-92.
(8.) Linares A, Cortellini P, Lang NP et al. Guided tissue regeneration/deproteinized bovine bone mineral or papilla preservation flap alone for treatment of intrabony defects. II: radiographic predictors and outcomes. J Clin Periodontol 2000;33:351-358.
(9.) Aichelmann-Reidy ME, Reynolds MA. Predictability of clinical of outcomes following regenerative therapy in intrabony defects. J Periodontol 2008;79:387-393.
(10.) Sculean A, Schwarz F, Chiantella GC et al. Five-year results of a prospective, randomized, controlled study evaluating treatment of intrabony defects with a natural bone mineral and GTR. J Clin Periodontol 2007;34:72-7.
(11.) Paolantonio M, Perinetti G, Dolci M et al. Surgical treatment of periodontal intrabony detects with calcium sulfate implant and barrier versus or open flap debridement alone: a 12-month randomized controlled clinical trial. J Periodontol 2008:79:1,886-93.
(12.) Luepke PG, Mellonig JT, Brunsvold MA. A clinical evaluation of a bioresorbable barrier with and without decalcified freeze-dried bone allograft in the treatment of molar furcations. J Clin Periodontol 1997;24:440-446.
(13.) Garrett S, Poison AM, Stoller NH et al. Comparison of a bioabsorbable GTR barrier to a non-absorbable barrier in treating human class II furcation defects. A multi-center parallel design randomized, single-blind trial. J Periodontol 1997;68:667-675.
(14.) Eickholz P, Kim TS, Holle R, Hausmann E. Long-term results of guided tissue regeneration therapy with non-resorbable and bioabsorbable barriers. I. Class II furcations. J Periodontol 2001;72:35-42.
(15.) Bowers CM, Schallhorn RG, McClain PK et al. Factors influencing the outcome of regenerative therapy in mandibular Class II furcations: Part I.J Periodontol 2003;74:1,255-68.
(16.) Machtei EE. Schallhorn RG. Successful regeneration ot mandibular Class II furcation defects: an evidence-based treatment approach. Int J Periodontics Restorative Dent 1995;15:146-67.
(17.) Miron RJ, Sculean A, Cochran DL et al. Twenty years of enamel matrix derivative: the past, the present and the future. J Clin Periodontol 2016;43:668-83.
(18.) Esposito M, Grusovin MG, Papanikolaou N, et al. Enamel matrix derivative (Emdogain) for periodontal tissue regeneration in intrabony defects. Cochrane Database Syst Rev 2009;CD003875.
(19.) Koop R, Merheb J, Quirynen M. Periodontal regeneration with enamel matrix derivative in reconstructive periodontal therapy: a systematic review. J Periodontol 2012;83:707-20.
(20.) Lekovic V, Camargo PM, Weinlaender M, et al. A comparison between enamel matrix proteins used alone or in combination with bovine porous bone mineral in treating intrabony periodontal defects in humans. J Periodontol 2000:71:1,110-6.
(21.) Velasquez-Plata D, Scheyer ET, Mellonig JT. Clinical comparison of an enamel matrix derivative used alone or in combination with a bovine-derived xenograft for the treatment ot periodontal osseous defects in humans. J Periodontol 2002;73:433-40.
(22.) Sculean A, Pietruska M, Arweiler NB, et al. Four-year results of a prospective-controlled clinical study evaluating healing of intra-bony defects following treatment with an enamel matrix protein derivative alone or combined with bioactive glass. J Clin Periodontol 2007;34:507-13.
(23.) Cortellini P, Tonetti MS. Clinical performance of a regenerative strategy for intrabony defects: scientific evidence and clinical experience. J Periodontol 2005;76:341-350.
(24.) Stavropoulos A, Wikesjo UM. Growth and differentiation factors for periodontal regeneration: a review on factors with clinical testing. J Periodontal Res 2012;47:545-53.
(25.) Lynch SE, de Castilla GR, Williams RC et al. The effects of short-term application of a combination ot platelet-derived and insulin-like growth factors on periodontal wound healing. J Periodontol 1991;62:458-467.
(26.) Nevins M, Camelo M, Nevins ML et al. Periodontal regeneration in humans using recombinant human platelet-derived growth factor-BB (rhPDGF-BB) and allogenic bone. J Periodontol 2003:74:1,282-92.
(27.) King GN, Hughes FJ. Bone morphogenetic protein-2 stimulates cell recruitment and cementogenesis during early wound healing. J Clin Periodontol 2001;28:465-75.
(28.) Kwon DH, Bisch FC, Herald RW et al. Periodontal wound healing/regeneration following the application ot rhGDF-5 in a beta-TCP/PLGA carrier in critical-size supra-alveolar periodontal defects in dogs. J Clin Periodontol 2010;37:667-74.
(29.) Moore YR, Dickinson DP, Wikesjo UM. Growth/differentiation factor-5: a candidate therapeutic agent for periodontal regeneration? A review of pre-clinical data. J Clin Periodontol 2010;37:288-98.
(30.) Kitamura M, Akamatsu M, Machigashira M et al. FGF-2 stimulates periodontal regeneration: results ot a multi-center randomized clinical trial. J Dent Res 2011;90:35-40.
(31.) Kitamura M, Akamatsu M, Kawanami M et al. Randomized placebo-controlled and controlled non-inferiority Phase III trials comparing trafermin, a recombinant human fibroblast growth factor 2, and enamel matrix derivative in periodontal regeneration in intrabony defects. J Bone Miner Res 2016;31:806-14.
Georgios Chatzopoulos, D.D.S. (*)
(*) Dr. Georgios Chatzopoulos is a resident in Periodontology, Department of Developmental and Surgical Sciences, Division of Periodontology, University of Minnesota School of Dentistry, Minneapolis, Minnesota 55455. Email is chat005@umn.edu