When the heart muscle doesn’t get enough oxygen-rich blood, discomfort, or chest pain occurs. This is pain called angina.
Angina isn’t a disease; it is a primary symptom of a heart problem like coronary heart disease or coronary microvascular disease.
The pain or discomfort experienced can be a burning or fullness sensation, or it may feel more like a generalized pressure like something is compressing the chest.
Besides, pain may occur in the arms, shoulder, jaw, back, or neck, and it may be accompanied by shortness of breath.
If you are experiencing these symptoms, please call 911 immediately as they may be a sign of a heart attack.
Women may experience angina differently than men; the heart pain may be more stabbing in nature,
and it may be accompanied by abdominal pain, shortness of breath, and discomfort in the neck, jaw, or back.
Certain non-cardiac conditions like COPD and diabetes may increase your risk of developing angina symptoms.
When you experience chest pains or discomfort, even when mild, you should be seen by a physician.
This discomfort may be a sign of a serious underlying heart condition like atherosclerosis that can impede the flow of oxygen-rich blood to your heart.
Conventional treatment depends on the type of angina you are experiencing and the underlying cause and may range from medications and observation to surgical intervention.
Natural therapies can help prevent recurring chest pains, and they may help to lower blood pressure and cholesterol, two prominent risk factors for heart disease.
What Is Angina?
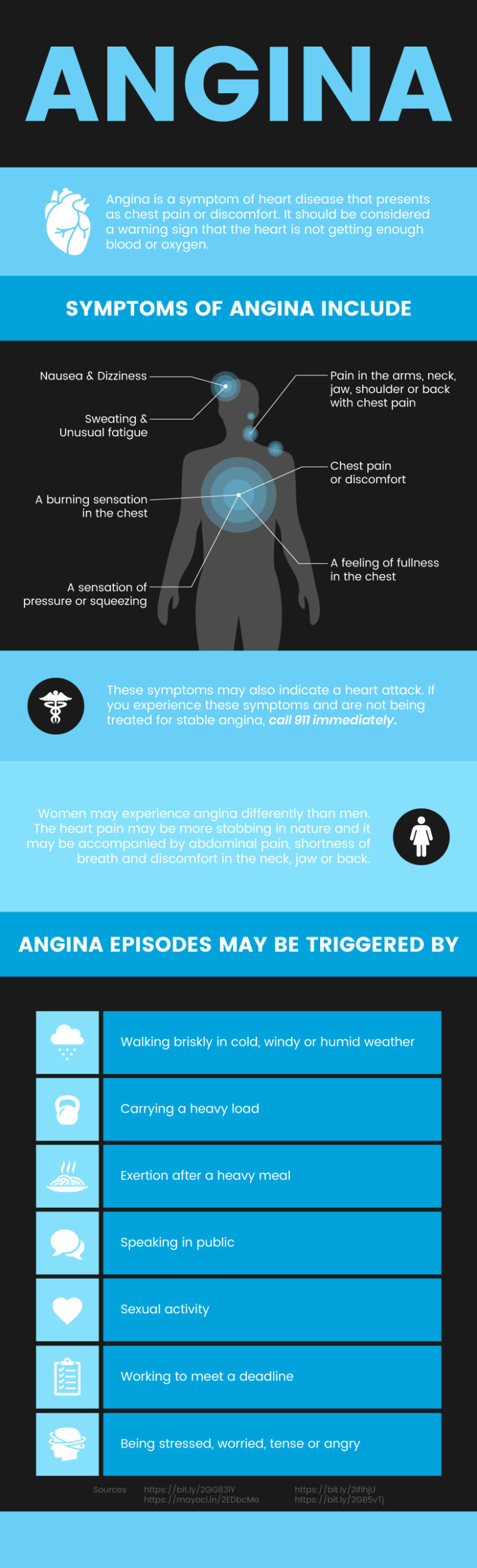
In simple terms, angina is a symptom of heart disease that presents as chest pain or discomfort.
It should be considered a warning sign that the heart is not getting enough blood or oxygen.
This can be a result of narrowed or blocked arteries that impede blood flow. There are four types of angina: Unstable, Stable, Variant, and Microvascular.
Unstable
Unstable angina is a medical emergency; call 911 if you have an episode of unstable angina. Hallmarks of this type include:
- Chest pains that occur while at rest
- Unexpected angina episodes
- Chest pains that last 30 minutes or longer
- Angina symptoms that do not respond to medication or rest
- A change in the typical pattern of stable angina
Stable
This is the most common form of angina, and it is also referred to as angina pectoris. It’s often a chronic condition. This type’s hallmarks include:
- Chest pains occur during physical exertion and exercise
- Anxiety is similar to previous angina events
- Angina episodes last five minutes or less
- Symptoms disappear after medication or rest
- Pain and discomfort can be predicted
- Pain may feel like indigestion or gas
- Pain may radiate to other areas, including arms, back or neck
- May be triggered by emotional stress, exposure to hot or cold weather, or smoking.
Variant
Also known as Prinzmetal’s Angina, it’s a more rare form of chronic angina, accounting for only 2 out of 100 cases.
A spasm causes it in the coronary arteries, not a blockage. This type presents:
- When at rest, often in the middle of the night
- As a response to stress
- With symptoms that are often severe
- With chest pains that are relieved with medication
Microvascular Angina
It’s usually a symptom of coronary microvascular disease, a disease that affects the smallest coronary artery blood vessels.
Spasms can occur, causing less blood flow to the heart. Microvascular angina may:
- Present with more severe and intense chest pains
- Last longer than other types of angina
- Occur during times of mental or emotional stress
Angina Signs & Symptoms
Symptoms of angina include:
- Chest pain or discomfort
- Pain the arms, neck, jaw, shoulder or back with chest pain
- A burning sensation in the chest
- An impression of pressure or squeezing
- A feeling of fullness in the chest
- Sweating
- Unusual fatigue
- Nausea
- Dizziness
These symptoms may indicate a heart attack. If you experience these symptoms and are not being treated for stable angina, call 911 immediately.
Causes & Risk Factors
Stable angina and unstable angina are caused when one or more of the coronary arteries are narrowed or blocked, and blood flow to the heart is not adequate.
Prinzmetal’s angina and microvascular angina are caused by spasms in arteries that feed the soul, resulting in heart pain and discomfort.
Recognized risk factors for angina include:
Angina episodes may be triggered by
- Walking briskly in cold, windy or humid weather
- Carrying a heavy load
- Exertion after a heavy meal
- Speaking in public
- Sexual activity
- Working to meet a deadline
- Being stressed, worried, tense or angry
Angina Diagnosis
Diagnosing angina requires a full medical history and physical exam. Also, many tests may be ordered to confirm the diagnosis. These include:
Blood Tests: Often, one of the first tests ordered, a simple blood test may reveal a heart attack. When your heart is damaged, your blood may inform certain heart enzymes that have leaked into your bloodstream.
Electrocardiogram (ECG): This non-invasive diagnostic tool records electrical signals of the heart in a pattern. These patterns may reveal problems of blood flow or if you have a heart attack.
Echocardiogram: Another non-invasive diagnostic procedure, the echocardiogram uses sound waves to produce images of the heart.
These images may help doctors to identify the cause of chest pains and identify areas of the heart muscle that are damaged.
Chest X-ray: X-rays of both the heart and lungs are often ordered to look for the root cause of the angina symptoms.
Cardiac CT Scan: This test is ordered to give your doctor multiple pictures of your heart and chest.
A cardiac CT scan can show if your heart is enlarged and if arteries feeding the soul are narrowed or blocked.
Cardiac MRI: This MRI provides detailed images of the heart, its structure, and blood vessels, allowing your doctor to identify issues causing your chest pains.
Stress Test: If you have stable angina, a stress test may be ordered to see if chest pains can be induced.
The test may be conducted while riding a stationary bike or walking on a treadmill.
During the trial, ECG readings and your blood pressure are monitored. For those unable to exercise, a drug may be administered to stimulate exercise.
Nuclear Stress Test: Similar to the stress test but with the addition of a radioactive substance injected into the bloodstream.
This substance is visible in images, and as it travels, any blocked or narrowed arteries where the content can’t pass will become apparent.
Coronary Angiography: With this procedure, a dye is injected into the blood vessels of your heart, and X-rays then reveals a detailed look at your heart and blood vessels.
Conventional Treatment
The goal is to reduce the frequency and severity of angina and lower your overall risk of a heart attack and death.
Treatment may include one or more of the following medications or procedures.
Nitrates: Commonly prescribed for angina, nitrates help to relax and widen the blood vessels, which allows blood to flow more freely to the heart muscle.
Nitrates can be used on a preventative basis longterm, or they can be taken at the onset of chest pains or discomfort.
Aspirin: Low-dose aspirin is often prescribed to help prevent blood clots.
Plavix, Efficient, or Brilliant: These are clot-preventing drugs that are often prescribed for angina patients who cannot take aspirin.
They are commonly prescribed to reduce the rate of strokes, myocardial infarctions, and unstable angina.
Beta-Blockers: These drugs help blood vessels relax, improving blood flow, and thereby reducing angina symptoms.
They work by blocking epinephrine, so the heart beats slower, lowering blood pressure.
Beta-blockers may also be prescribed for high blood pressure, arrhythmia, migraines, and heart failure.
Statins: These drugs are used to lower blood cholesterol, and, according to the Mayo Clinic,
statins may help your body reabsorb cholesterol in the artery walls, helping to prevent blockages in the blood vessels.
Calcium Channel Blockers: These drugs widen and relax the blood vessels, increasing blood flow to the heart. They may reduce the number of angina episodes or prevent it.
Blood Pressure Medications: For patients with high blood pressure, ACE inhibitors, or ARBs will likely be prescribed to bring your blood pressure to a healthy state.
Ranexa (Ranolazine): This drug is often prescribed alongside other angina medications and is commonly used in the treatment of angina pectoris.
Ranexa works by reducing the flow of calcium into the cells, helping the heart relax, and improving blood flow to the heart muscle.
Angioplasty with Stents: When heart arteries are clogged, a surgeon will insert and inflate a balloon at the site of the clog to widen the highway.
A small wire mesh tube may be placed to help keep the road open. This surgery can improve chest pains and shortness of breath.
Coronary Artery Bypass Surgery: This surgery is used for both stable and unstable angina that hasn’t responded to other treatments.
In this surgery, a healthy vein from another part of your body is harvested and then placed to bypass a blocked or narrowed artery.
This surgery increases blood flow to the heart muscle and may reduce or eliminate angina related chest pains.
8 Natural Ways to Help Relieve Angina
1. Quit Smoking
If you smoke, quit smoking. Smoking increases your risk for several kinds of cancer and chronic obstructive pulmonary disease (COPD), as well as atherosclerosis and coronary heart disease, both of which can cause angina chest pains.
Mind-body practices can help you overcome your nicotine addiction.
One of the most promising is yoga. Yoga and smoking are similar in that they both involve deep breathing and relaxation.
Researchers have found that yoga reduces heart rate and blood pressure while increasing pulmonary function and inducing a relaxed sense of well-being.
Find the right yoga practice for you and do it two to three times a week as an effective smoking cessation practice.
2. Acupuncture
Used for thousands of years for a wide range of ailments, acupuncture may help relieve chest pain associated with angina.
In a meta-analysis of nine randomized-controlled trials published in the International Journal of Clinical and Experimental Medicine, researchers indicate that acupuncture can help relieve angina symptoms,
including chest pains in patients with stable angina pectoris.
And, perhaps more importantly, acupuncture significantly increased the effectiveness of clinical curative treatments. Researchers encouraged more clinical trials.
3. CoQ10
For heart health, and specifically for angina symptoms, take 60 milligrams to 100 milligrams of CoQ10 daily.
Coenzyme Q10 is needed by every cell in the human body. It is known for protecting the blood vessels and heart from oxidative stress.
And, it may help lower the heart’s oxygen demand while improving its efficiency.
A bonus side effect for cardiac patients — it may help to reduce blood pressure and improve exercise performance for those with stable angina, according to a small study published in the American Journal of Cardiology.
4. L-Carnitine
Take 1,000 milligrams, twice a day of a high-quality L-carnitine supplement, to help relieve angina symptoms.
In a systematic review and meta-analysis published in Mayo Clinic Proceedings, L-carnitine is associated with a 27 percent reduction in mortality, a 65 percent reduction in ventricular arrhythmias, and a 40 percent reduction in angina symptoms for those experiencing a myocardial infarction.
Researchers encourage more extensive randomized controlled trials to support L-carnitine for cardiovascular disease.
5. Fish Oil
If you have heart problems, low HDL cholesterol levels, and high triglycerides, take fish oil supplements to help keep blood flowing properly.
In a multi-center, double-blind, placebo-controlled trial, patients with acute myocardial infarction were treated with high doses of omega-3 fatty acids for six months or with a placebo.
Patients treated with omega-3 fatty acids experienced an overall reduction of adverse cardiac events, including myocardial fibrosis, systemic inflammation, and ventricular remodeling.
6. Start Exercising
Even mild and moderate exercise can help you in many ways when you have angina.
Not only is exercising a great way to reduce stress, a recent study published in the journal Scientific Reports indicates that rehabilitation exercise after a cardiac event experience improvement in angina-related chest pains and enjoyed longer exercise time and better exercise tolerance.
Be sure to talk with your doctor first before starting an exercise program.
Of course, if you have been diagnosed with a cardiac condition, you must talk to your medical team before undertaking any sort of exercise program.
Building up your heart’s strength is essential, and as exercise and exertion can cause angina, taking it slow is a must.
You may want to start by taking a short walk on a flat, even surface for 10 to 15 minutes.
As you build endurance (and get clearance from your cardiac team), you can add both intensity and distance. In addition to walking, tai chi, yoga, and Pilates can be great options.
7. Reduce Stress
Stress and anxiety can induce chest pains in those with angina pectoris.
The Mayo Clinic recommends that people with angina find a way to relax and avoid stress as much as possible.
Learning to adapt natural stress relievers into your daily routine is vital for overall heart health.
Meditation, cognitive behavioral therapy, deep breathing exercises, writing in a journal, and even spending more time outdoors or being social may be just the impetus you need to induce relaxation.
8. EECP
EECP or “enhanced external counterpulsation,” is a non-invasive procedure that is used for a variety of cardiac conditions, including angina.
Most often conducted in clinics and hospital environments, it is now also offered at a range of medical spas and other facilities.
In conventional cardiac treatment, it is often used as a last resort when surgical options have failed or when patients aren’t a candidate for surgery.
But, research shows that it may be an effective, non-invasive treatment that is also cost-effective.
EECP works to relieve heart conditions, including angina, by creating new blood vessel branches or opening narrowed or blocked vessels — essentially creating a natural bypass. The process isn’t quick, but there are no known risks or adverse side effects.
However, the greatest challenge of EECP is that it takes a commitment of 35 hours or more over seven weeks.
During a session, you are situated in a relaxing position, and electrodes are connected to an ECG machine.
Then, large cuffs are strapped around your calves, thighs, and buttocks.
The cuffs (think blood pressure cuff) firmly compress these areas by inflating and deflating in an offbeat of your natural heart rhythm.
This pushes oxygen-rich blood to the heart at the moment it is relaxed.
The Cleveland Clinic reports that patients who undergo EECP have less need for angina medication, experience a decrease in angina symptoms, and can enjoy activities without chest pains.
Some insurance companies may pay for this treatment if recommended by a cardiologist.
This non-invasive, non-surgical treatment may be worth fighting for if you have stable or unstable angina or other cardiac problems.
In addition to angina and cardiovascular disease, it is currently being studied for its effectiveness for diabetes, atherosclerosis, cognitive impairment, muscle tightness, erectile dysfunction, and more.
Precautions
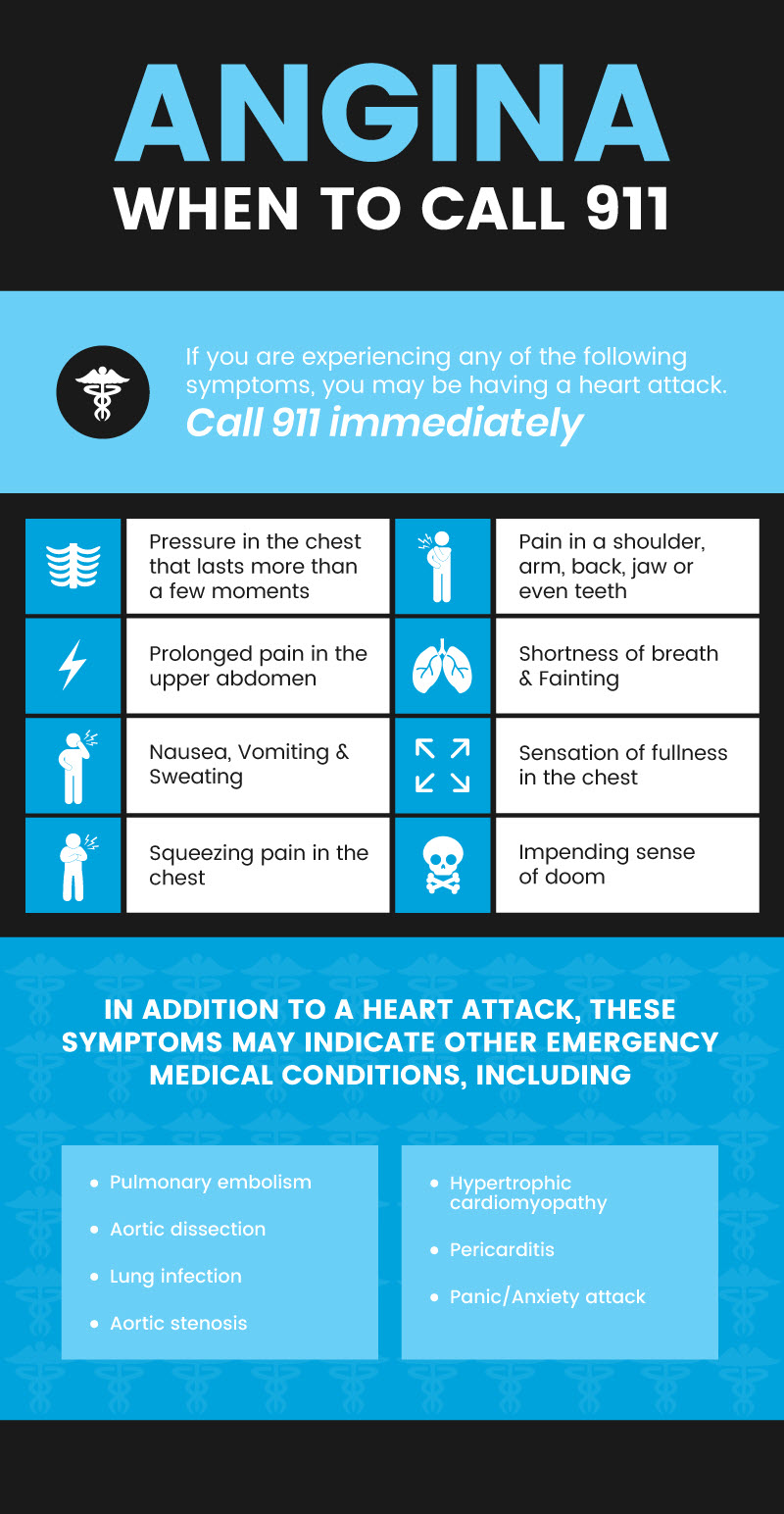
Angina should be considered a warning sign of a heart condition. If you are experiencing any of the following symptoms, you may be having a heart attack. Call 911 immediately.
- Pressure in the chest that lasts more than a few moments
- The sensation of fullness in the chest
- Squeezing pain in the chest
- Pain in a shoulder, arm, back, jaw or even teeth
- Prolonged pain in the upper abdomen
- Shortness of breath
- Sweating
- Fainting
- Nausea
- Vomiting
- The impending sense of doom
In addition to a heart attack, these symptoms may indicate other emergency medical conditions including (1)
Angina Key Points
- Angina is a symptom, or warning sign, of cardiovascular disease and presents as chest pains, tightness, or discomfort.
- When blood flow is impaired due to a clogged artery or narrowed artery, chest pains can occur.
- Women may experience angina differently than their male counterparts as the pain may be more stabbing in nature and accompanied by abdominal pains, pains in the neck, jaw or back, and shortness of breath.
- Conventional treatment for angina focuses on the underlying cause and may range from observation and medication to surgical intervention.
- Natural treatments may help relieve symptoms and help to improve overall cardiovascular health.
8 Natural Treatments for Angina
1. If you smoke, quit.
2. Acupuncture may help relieve chronic stable angina symptoms.
3. Take 60 milligrams to 100 milligrams of CoQ10 daily for heart health and to reduce symptoms.
4. Take 1,000 milligrams of L-carnitine daily to relieve symptoms, including chest pains.
5. Take high-quality fish oil to improve cholesterol levels and cardiac health.
6. Start exercising (with physician approval). Start slowly with walking and add yoga, Pilates, or tai chi.
7. Reduce stress with natural stress relievers, including cognitive behavioral therapy, meditation, deep breathing exercise, or whatever helps you to de-stress.
8. Try EECP. Talk to your doctor to find out if you are a candidate for EECP to help relieve symptoms and improve cardiac health.