Amyotrophic lateral sclerosis (ALS)
Amyotrophic lateral sclerosis (ALS) known as a motor neuron illness that causes damage to certain neurons (nerve cells) in the brain and also the spinal cord that controls voluntary movement.
ALS is progressive, meaning it becomes worse over time. Eventually, the damage causes individuals with ALS to lose total control of their muscles.
Amyotrophic lateral sclerosis can occur either sporadically or in a familial (inherited) pattern.
ALS is also called Lou Gehrig’s disease. Gehrig was a great and beloved baseball player who played for many years with Babe Ruth on the New York Yankees.
He developed the disease in 1939, forcing him to retire from baseball and bringing international attention to the disease.
He had 26 years when he was diagnosed with ALS. In France, ALS is called Charcot’s disease after Jean-Martin Charcot, who described the disease in the 1860s.
Although it can occur at any age, Amyotrophic lateral sclerosis usually is diagnosed in people between the ages of 40 to 60.
There is also a juvenile-onset form of Amyotrophic lateral sclerosis with symptoms appearing in childhood.
The renowned physicist Stephen Hawking was diagnosed with this form of ALS when he was 21 years old.
Hawking famously lived with the disease for 55 years, dying in 2018. Juvenile-onset ALS is rare.
The ALS Association estimates that about 16,000 Americans are living with ALS at any given time.
Most occur in people with no family history of the disease, and it is 20% more common in men than in women.
DESCRIPTION
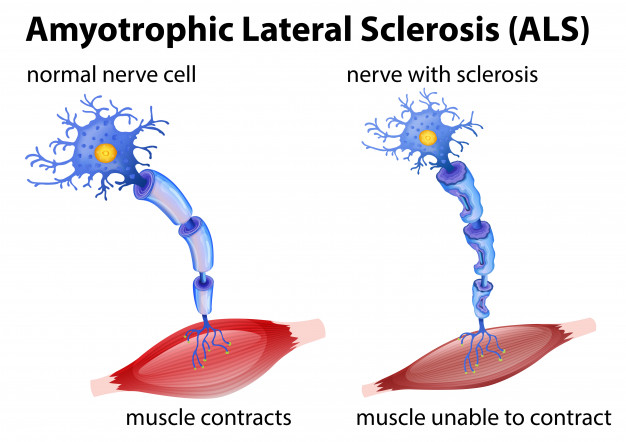
Motor neurons control voluntary movements (walking, grasping, etc.). These neurons are part of the neuromuscular system, which involves many neurons and muscle fibers throughout the body.
Motor neurons relay impulses within the brain, from the brain to the spinal cord, and from the spinal cord to the voluntary muscles.
Additional motor neurons in the brain can send signals directly to neurons within some specific muscles.
With ALS, these voluntary movements are affected when the motor neurons are damaged.
The damage continues, causing muscles to weaken, twitch, and waste away.
In addition to arms and legs, ALS eventually affects muscles involved in speaking, eating, and breathing. ALS rarely affects the senses of sight, hearing, smell, or touch.
CAUSES
For most cases of ALS, there is no known cause. Many researchers believed as of mid-2020 that ALS arises from a combination of environmental and genetic factors.
These factors cause changes (mutations) in certain genes. Most cases of ALS are the sporadic type, which means they occur randomly in individuals who have no known risk for the disease and no additional family member who has ALS.
Only about 5% to 10% of people with ALS have the familial type, which is linked to genetic factors.
Mutations in several genes are linked to juvenile and familial ALS, and each parent with an ALS-linked mutation has a 50% chance of passing on the mutation to their offspring.
SYMPTOMS AND DIAGNOSIS
The symptoms may vary from 1 person to another, but ALS begins with changes such as being unable to lift a glass or similar movement problems.
Early symptoms of ALS can include:
- tight, stiff muscles
- twitching muscles
- muscle cramps
- weak muscles
- trouble writing
- changes in speech such as pitch differences or slurring
- problems chewing or swallowing
The symptoms of juvenile ALS are similar but appear before a person turns 25 years old.
Some symptoms of ALS also are similar to those of other diseases, so doctors examine patients, discuss the symptoms, check neurological function (such as eye movement and reflexes), and order tests to determine the cause of the neuromuscular symptoms.
Electromyography (EMG) usually is the preferred test to check for ALS. An EMG can show problems with nerve and muscle function or the signal between nerves and muscles.
Stickers called surface electrodes are placed on the skin over the muscles being tested. The electrodes send signals back to the equipment that measures the speed and strength of the nerve signals under the sticker.
A needle might be inserted into the affected muscle to check electrical activity within the muscle. The test can be done in a physician’s office.
A nerve conduction study can be performed at the same time. In this study, a technician sends a mild electrical impulse to a nerve located under the patch to record how the nerve responds.
Other tests for Amyotrophic lateral sclerosis include a magnetic resonance imaging (MRI) exam or other imaging and lab tests to see if a different condition than ALS is causing the symptoms. Less often, doctors take a sample of spinal fluid or muscle tissue.
TREATMENT
There is no cure for Amyotrophic lateral sclerosis. Doctors treat the symptoms caused by damage to motor neurons to help patients have as much movement and independence as possible for as long as possible.
In mid-2020, doctors at the University of Texas-San Antonio announced results of a small study that showed promise in a new drug (phenylbutyrate-taurursodiol) that could slow the progression and extend patients’ lives.
A few medicines have been approved for use in people who have ALS. Riluzole (Rilutek) could reduce new damage to motor neurons and edaravone (Radicava) can slow the decline in function.
Neither drug can reverse the damage caused by Amyotrophic lateral sclerosis.
Additional medicines are prescribed to ease symptoms such as muscle cramps or stiffness.
LIVING WITH ALS
Having Amyotrophic lateral sclerosis requires ongoing and regular visits to a neurologist and other health professionals.
Doctors prescribe physical therapy to strengthen muscles not affected by ALS and help with movement.
Occupational therapy also assists by showing patients how to use equipment to help maintain independence.
Speech therapy helps improve problems with speaking and can train patients on special devices to help them communicate, such as eye-tracking technology.
A number of devices such as zipper pull, writing aids, and eating utensils help individuals with ALS perform daily functions.
In addition, ever-improving technology can help people living with ALS be more independent, including specially designed wheelchairs and computers to assist with speech communication.
As symptoms worsen, people who have ALS receive help with nutrition when eating becomes difficult.
Breathing support also becomes necessary, first just at night when individuals are lying down and eventually at all times.
Most people who have ALS eventually die of respiratory failure (the inability to breathe), often during sleep.
Research continues on determining the exact cause of ALS and how to treat the disease.
For example, scientists have been studying the use of stem cells in ALS to replace damaged motor neurons. Other therapies in the research stages could address the genes causing the disease.
Resources
Websites
“Amyotrophic lateral sclerosis.” MedlinePlus. August 4, 2020. https://medlineplus.gov/amyotrophiclateralsclerosis.html (accessed November 6, 2020).
“Amyotrophic Lateral Sclerosis (ALS).” Health Encyclopedia, University of Rochester Medical Center. https://www.urmc.rochester.edu/encyclopedia/content.aspx?ContentTypeID=85&ContentID=P00771 (accessed November 6, 2020).
“Amyotrophic lateral sclerosis (ALS) fact sheet.” National Institute of Neurological Disorders and Stroke. June 22, 2020. https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Amyotrophic-Lateral-Sclerosis-ALS-Fact-Sheet (accessed November 6, 2020).
“What Is ALS.” ALS Association. http://www.alsa.org/about-als/what-is-als.html (accessed November 6, 2020).
Organizations
ALS Association, 1300 Wilson Boulevard, Suite 600, Arlington, VA, 22209, (800) 782-4747, http://www.alsa.org/ .
Muscular Dystrophy Association, ALS Division, 161 N. Clark, Suite 3550, Chicago, IL, 60601, (800) 572-1717, Fax: (520) 529-5300, Resource Center@mdausa.org, https://www.mda.org.
National Institute of Neurological Disorders and Stroke, PO Box 5801, Bethesda, MD, 20824, (800) 352-9424, https://www.ninds.nih.gov.