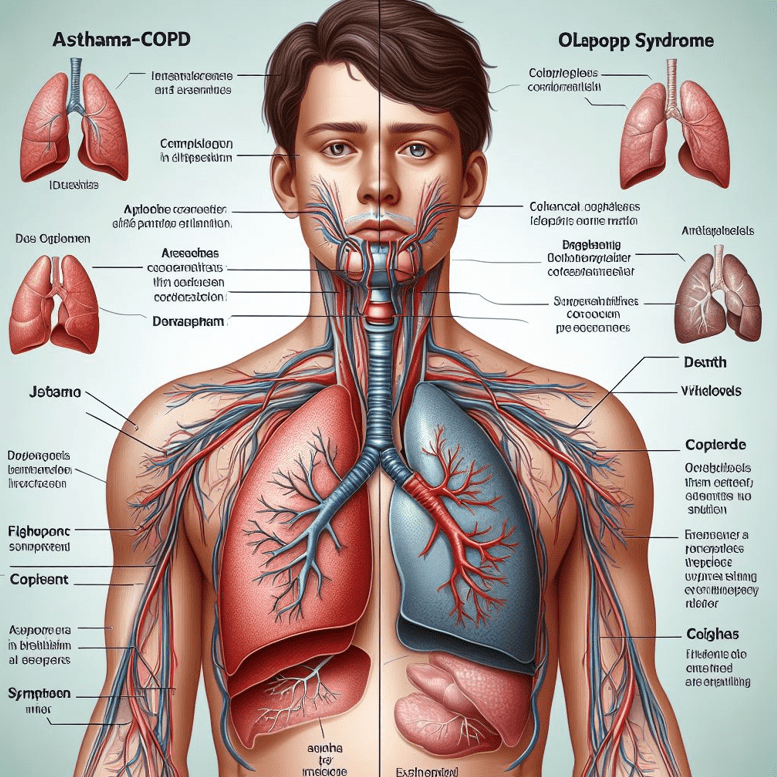
Asthma-COPD Overlap Syndrome (ACOS) is a medical condition that combines symptoms of both Asthma and Chronic Obstructive Pulmonary Disease (COPD). This complex respiratory disorder poses unique challenges for diagnosis and treatment. Understanding ACOS is crucial for healthcare professionals and patients alike, as it requires a tailored approach distinct from managing asthma or COPD alone.
Breathing difficulties can significantly impact daily life. For some individuals, these challenges stem from conditions like asthma or Chronic Obstructive Pulmonary Disease (COPD).
However, a distinct group experiences symptoms and characteristics of both, a condition known as Asthma-COPD Overlap Syndrome (ACOS). Understanding ACOS is vital because it requires a unique diagnostic approach and a carefully tailored treatment plan, which differs from managing asthma or COPD alone.
This article dives into what ACOS is, who it affects, how it’s diagnosed, and the best ways to manage it effectively.
What Exactly is Asthma-COPD Overlap Syndrome (ACOS)?
Asthma-COPD Overlap Syndrome (ACOS) isn’t simply having asthma and COPD at the same time; it refers to a specific clinical picture where patients exhibit features characteristic of both diseases. Key defining features often include:
-
Persistent Airflow Limitation: Like COPD, individuals with ACOS experience ongoing difficulty breathing out, which doesn’t completely resolve, even with medication.
-
Features of Asthma: Alongside the persistent limitation, there are often signs typical of asthma, such as significant variability in airflow (sometimes breathing is much better or worse than others) and airway hyperresponsiveness (airways are extra sensitive to triggers).
-
Mixed Airway Inflammation: The underlying inflammation in the airways often shows characteristics seen in asthma (like increased eosinophils, a type of white blood cell) and COPD (like increased neutrophils).
Distinguishing ACOS: While asthma typically involves reversible airflow obstruction often starting in childhood, and COPD involves largely irreversible obstruction linked primarily to smoking starting later in life, ACOS blends these profiles. Patients might have a history of asthma from a younger age and a significant smoking history, leading to this overlap presentation.
Who Gets ACOS? Prevalence and Risk Factors
Pinpointing the exact prevalence of ACOS is challenging due to varying diagnostic criteria. Still, estimates suggest that around 15-25% of patients initially diagnosed with either asthma or COPD may have ACOS. It appears to be more common as people age.
Key Risk Factors for Developing ACOS:
-
Smoking History: A history of cigarette smoking (current or former) is a significant risk factor, similar to COPD.
-
History of Asthma: A previous diagnosis of asthma, particularly if it started earlier in life.
-
Age: ACOS is more commonly diagnosed in adults over 40.
-
Environmental Exposures: Long-term exposure to air pollution, occupational dust, or chemicals can contribute.
-
Genetics: Certain genetic factors may predispose individuals to airway diseases.
The Underlying Biology: Pathophysiology of ACOS
Understanding ACOS requires looking at the mechanisms of both parent conditions:
-
Asthma Component: Characterized by chronic inflammation often driven by allergic responses and eosinophils. This leads to bronchoconstriction (tightening of airway muscles), mucus production, and swelling of the airway lining, causing reversible airflow obstruction.
-
COPD Component: Primarily caused by long-term exposure to irritants like cigarette smoke. This leads to damage to the air sacs (emphysema) and inflammation/narrowing of the small airways (chronic bronchitis), causing largely irreversible airflow limitation.
In ACOS, these processes coexist. Patients experience the chronic, irreversible damage associated with COPD alongside the variable inflammation and airway hyperresponsiveness typical of asthma. This complex mix results in the persistent yet sometimes variable symptoms seen in ACOS.
Recognizing the Signs: Symptoms of ACOS
Symptoms of ACOS can be variable and overlap significantly with both asthma and COPD, making diagnosis tricky based on symptoms alone. Common signs include:
-
Persistent Dyspnea: Ongoing shortness of breath, often worse with exertion.
-
Chronic Cough: May be dry or produce sputum (phlegm).
-
Wheezing: A high-pitched whistling sound during breathing, which can be variable.
-
Chest Tightness: A feeling of constriction or pressure in the chest.
-
Variable Symptoms: Patients might experience “good days and bad days,” more so than typically seen in COPD alone.
-
Frequent Exacerbations: Episodes where symptoms suddenly worsen (flare-ups) may be more common or severe.
Diagnosing ACOS: A Complex Puzzle
Because symptoms overlap, diagnosing ACOS requires a thorough evaluation. There isn’t one single test; diagnosis relies on piecing together evidence from various sources:
-
Detailed Medical History: Discussing symptoms (onset, variability, triggers), history of allergies or asthma (especially in childhood), smoking history (pack-years), family history of respiratory diseases, and exposure to pollutants is crucial.
-
Physical Examination: Listening to the lungs for wheezing or other abnormal sounds.
-
Lung Function Tests (Spirometry): This is essential. It measures how much air you can breathe in and out, and how quickly. In ACOS, spirometry typically shows persistent airflow limitation (like COPD) but may also show a significant improvement in airflow after inhaling a bronchodilator medicine (a feature more typical of asthma).
-
Imaging Studies: Chest X-rays or CT scans can help identify features of emphysema or airway thickening (seen in COPD) and rule out other lung conditions.
-
Biomarkers and Allergy Testing: Blood tests (checking for eosinophil counts) or sputum analysis can indicate the type of inflammation present (eosinophilic inflammation suggests an asthma-like component). Allergy skin testing might be done if allergies are suspected triggers.
-
Differential Diagnosis: Doctors must carefully rule out other conditions that can cause similar symptoms, such as heart failure, bronchiectasis, or other lung diseases.
Diagnosing ACOS often involves confirming persistent airflow limitation while also identifying features strongly suggestive of asthma.
Managing ACOS: A Tailored Treatment Approach
Treatment for ACOS aims to combine the most effective strategies from both asthma and COPD management, personalized to the individual patient’s specific features and symptom severity.
-
Lifestyle Modifications:
-
Smoking Cessation: Absolutely paramount. Stopping smoking is the single most effective action to slow disease progression and improve outcomes. Support programs and medications can help.
-
Avoid Triggers: Identifying and avoiding known asthma triggers (allergens, irritants) is important.
-
Physical Activity: Regular, appropriate exercise can improve breathing efficiency and quality of life.
-
-
Medications: Most patients require inhaled medications.
-
Bronchodilators: These relax airway muscles to make breathing easier.
-
Short-acting beta-agonists (SABAs): Used for quick relief of sudden symptoms.
-
Long-acting beta-agonists (LABAs) & Long-Acting Muscarinic Antagonists (LAMAs): Used regularly to control symptoms and prevent flare-ups. Combinations (LABA/LAMA) are common.
-
-
Inhaled Corticosteroids (ICS): These are crucial for managing the underlying inflammation, particularly the asthma component. Most ACOS patients benefit from an ICS, often in combination with a LABA (ICS/LABA). The dose may need adjustment based on inflammatory markers like eosinophils.
-
Combination Inhalers: Many patients use inhalers containing multiple medications (e.g., ICS/LABA, ICS/LABA/LAMA) for convenience and effectiveness.
-
-
Pulmonary Rehabilitation: A structured program including exercise training, disease education, breathing techniques, and psychological support. It significantly improves exercise tolerance, reduces symptoms, and enhances quality of life.
-
Vaccinations: Annual flu shots and pneumococcal vaccinations are vital to prevent respiratory infections, which can cause severe exacerbations.
-
Managing Flare-ups (Exacerbations): Patients need an action plan for worsening symptoms, which usually involves increasing reliever medication use and potentially starting oral corticosteroids or antibiotics under medical guidance.
Challenges in Living With and Managing ACOS
Living with and treating ACOS presents unique hurdles:
-
Diagnostic Difficulty: Overlapping symptoms can delay accurate diagnosis.
-
Treatment Complexity: Finding the right combination and dosage of medications can take time and requires careful monitoring.
-
Managing Comorbidities: Patients with ACOS often have other health issues (heart disease, osteoporosis, anxiety/depression) that need concurrent management.
-
Adherence: Sticking to a potentially complex medication regimen and lifestyle changes requires ongoing patient education and support.
-
Predicting Response: How individuals respond to specific treatments can be more variable than in asthma or COPD alone.
Living Well with ACOS
Despite the challenges, effective management can significantly improve the quality of life for individuals with ACOS. Key strategies include:
-
Adhering to Treatment: Taking medications exactly as prescribed.
-
Using Inhalers Correctly: Ensuring proper technique maximizes medication delivery.
-
Following an Action Plan: Knowing what to do when symptoms worsen.
-
Staying Active: Engaging in safe levels of physical activity.
-
Seeking Support: Connecting with healthcare providers and potentially patient support groups.
When to Seek Medical Advice
It’s essential to consult a healthcare professional if you experience persistent respiratory symptoms like shortness of breath, chronic cough, or wheezing. If you have been diagnosed with asthma or COPD but your symptoms are not well-controlled or seem unusual, discuss the possibility of ACOS with your doctor. Seek immediate medical attention if you experience severe shortness of breath, confusion, or bluish lips/fingernails.
Conclusion
A Unique Condition Requiring Personalized Care
Asthma-COPD Overlap Syndrome (ACOS) is more than just co-existing asthma and COPD; it’s a distinct clinical entity requiring careful diagnosis and a personalized management strategy. By combining therapies effective for both conditions, focusing on smoking cessation, and incorporating pulmonary rehabilitation and preventative measures like vaccinations, individuals with ACOS can achieve better symptom control and maintain a higher quality of life. Ongoing research continues to shed light on ACOS, paving the way for even more targeted and effective treatments in the future.
[Disclaimer: This article is intended for informational purposes only and does not constitute medical advice. The information herein is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay seeking it because of something you have read in this article.]
References
-
Research Review on ACOS (via PubMed Central / NIH):
-
Bateman ED, et al. The Asthma-COPD Overlap Syndrome: Towards a Revised Approach (2015)
-
Description: This article, available through the National Institutes of Health’s PubMed Central archive, provides a detailed clinical review and discusses approaches to understanding and diagnosing Asthma-COPD Overlap Syndrome.
-
-
Global Initiative Guidelines (GOLD/GINA):
-
Global Initiative for Chronic Obstructive Lung Disease (GOLD) Reports
-
Description: The GOLD reports represent internationally recognized, evidence-based guidelines for managing and preventing COPD. While not solely focused on ACOS, their documents often address the overlap and diagnostic considerations, reflecting expert consensus.
-
Example State Public Health Information (Montana DPHHS):
-
Description: An example of how state-level public health departments provide information on ACOS for public awareness and surveillance. This demonstrates government recognition of the condition.
-