Dysthymia — also known as persistent depressive disorder, chronic depression, or dysthymic disorder — is a long-lasting form of clinical depression.
It often lasts for several years at a time, with symptoms coming and going, changing from day to day and week to week.
Many people with dysthymia or “dysthymic mood” can benefit from both talk therapy and medical treatment.
With changes to lifestyle and a strong understanding of what helps you personally cope with dysthymia,
you can also use natural approaches to boost your mood and manage your symptoms.
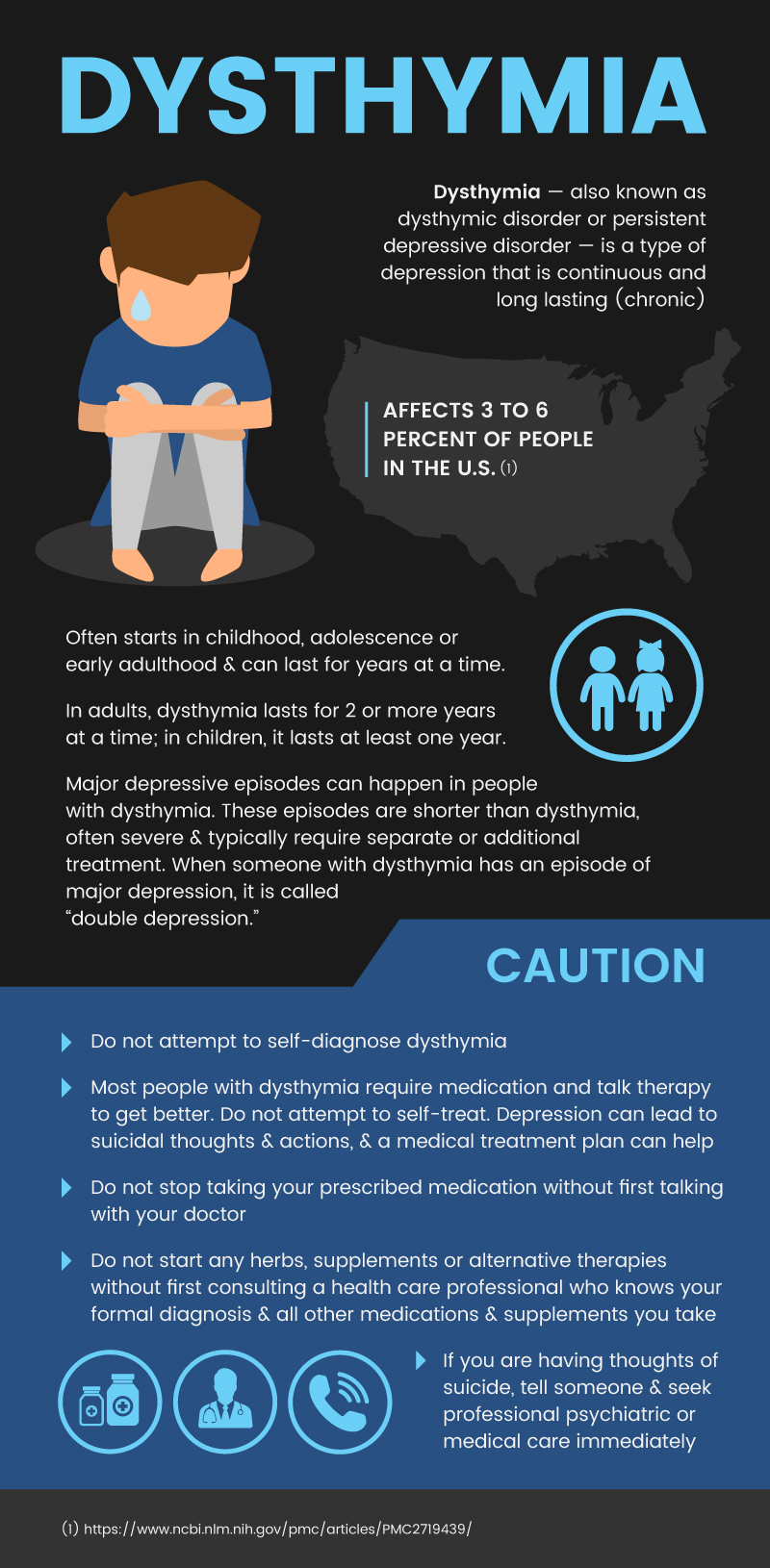
What Is Dysthymia?
Dysthymia — also known as a dysthymic disorder or persistent depressive disorder — is a type of depression that is continuous and long-lasting (chronic).
It used to be considered a milder diagnosis than major depression, but it is now known to have serious impacts on people’s lives and their ability to function normally.
The condition affects 3 to 6 percent of people in the U.S.
Dysthymia often starts in childhood, adolescence, or early adulthood and can last for years at a time.
It puts people at risk for other personality disorders and substance abuse and can cause problems with relationships, school or work, and day-to-day activities.
In adults, dysthymia lasts for two or more years at a time; in children, it lasts at least one year. People with dysthymia have fluctuations in how they feel.
They may not always be so depressed they can’t function, but they do often have symptoms of depression that can make it hard for them to enjoy activities or feel good about themselves or their lives.
At any given time, the symptoms may be mild, moderate, or severe.
People with dysthymia may have breaks in a depressed mood, but these breaks don’t last longer than two months at a time.
Dysthymia versus depression of other types
- Unlike seasonal affective disorder (SAD), which comes and goes with the seasons and also has variations in intensity, dysthymia does not depend on light exposure and time of year.
- Major depressive episodes can happen in people with dysthymia. However, these episodes are shorter than dysthymia, often severe, and typically require separate or additional treatment. When someone with dysthymia has an episode of major depression, it is called “double depression.”
- Post-partum depression is a type of depression that sometimes occurs after a woman gives birth. It may share symptoms with dysthymia but usually does not last as long. However, dysthymia can begin around the time of childbirth (called peripartum onset dysthymia).
- Dysthymia can have different features in different people, including symptoms of anxiety, melancholy, psychosis, and more.
Signs & Symptoms
Symptoms of this disorder are similar to signs and symptoms of depression in general. To be diagnosed with this particular disorder, you must have these dysthymia symptoms:
- Depressed mood (feeling down and uninterested in regular activities) for most of the day on most days
- lasting two years in adults and one year in children and adolescents
- irritability may be more prominent than depressed mood for children and adolescents
In addition, you must have two or more of these symptoms:
- Poor appetite or overeating
- Sleeping too much or not enough
- Feeling very tired or physically exhausted
- Low self-esteem
- Not being able to concentrate
- Trouble making decisions
- Feeling hopeless
As with other types of depression, you may also have excessive anger or irritability, feelings of guilt or anxiety, a desire to avoid social activities, and a decrease in productivity.
Dysthymia Causes & Risk Factors
There is no single cause known for dysthymia. It appears to be more common in families that have others affected by depression.
This suggests there is some genetic component. However, there is no known gene or biological abnormality that causes dysthymia.
Some people have levels of interleukin-1 and serotonin that are not normal.
Interleukin-1 has a role in inflammation and immune function. Serotonin is involved in communication between cells in the nervous system that is connected to mood and social functioning.
Risk factors for dysthymia include:
- Family members with any type of depressive disorder
- Stress in childhood or adulthood
- Isolation and lack of support
- Long-term medical problems
- Poor coping strategies
- Loss of a loved one or other traumatic event
- Poor self-esteem, negativity
- Diagnoses with another personality disorder, such as antisocial behavior, dependency or schizophrenia
Conventional Treatment
As with most mental health disorders, treatment for dysthymia varies from person to person.
The type of treatment that works for you will depend on how severe your symptoms are, how willing you are to work on your emotional symptoms,
and whether you are interested in dealing with situations in your life that impact your health.
Medical treatment will also depend on whether you have other health problems, what medication(s) you have tried in the past, and how your body reacts to each drug.
As for other types of depression, dysthymia treatment usually combines talk therapy (psychotherapy) and medication.
The types of medication used to treat dysthymia usually include the following antidepressants:
- Selective serotonin reuptake inhibitors (SSRIs)
- Serotonin and norepinephrine reuptake inhibitors (SNRIs)
- Tricyclic antidepressants (TCAs)
- Monoamine oxidase inhibitors (MAOIs)
- Noradrenergic drugs, such as mirtazapine, nefazodone, venlafaxine, duloxetine, and bupropion
Dysthymia: 7 Natural Ways to Improve Your Mood
Dysthymia is a serious mental health condition that should not be treated with alternative medicine alone.
However, there are many natural ways to relieve depression that may boost your mood, reduce your stress, and help you cope with your symptoms.
Natural ways to improve your mood and manage dysthymia symptoms include:
- Exercise
- Proactively manage your stress
- Get therapy
- Stay socially engaged
- Eat to support your mental health
- Consider aromatherapy
- Ask about supplements and herbs
-
Exercise
There is substantial evidence that exercise improves mood.
This is probably because exercise boosts the amount of tryptophan and serotonin in your brain.
These natural compounds both support improved mood. According to a study looking at a large body of research on exercise and depression:
- Structured exercise can relieve symptoms of clinical depression.
- Exercise may result in a happier mood.
- Improvements can last as long as three to 12 months after a training program ends.
- Benefits may be similar between aerobic exercise (running, walking, swimming) and resistance or strength training (weight lifting, stretching).
- Exercise may be just as beneficial as talk therapy.
- For some people, exercise may work just as well as medication to reduce symptoms of depression in the short term, and it may have longer-lasting effects.
Before you start an exercise program, talk with a health care professional. Here are some tips for using exercise to treat depression symptoms:
- Start slowly and pick something you like.
- Walking or jogging as little as 20 minutes per day, three days per week may be enough to significantly relieve symptoms and boost mood.
- Exercise doesn’t have to be super-intense or lengthy for you to get a benefit.
- Have a back-up plan for days with bad weather or when it is not safe or comfortable to exercise outside.
- Choose a place and time to actually schedule exercise into your day. Make sure it is convenient for you.
- Track your progress using an exercise log, pedometer, or a series of weekly or monthly goals.
-
Proactively manage your stress
Proactively managing your stress can help stop problems before they start.
By relieving sources of stress, you have less to upset you.
According to the Mayo Clinic, you can improve your ability to relax and manage stress by meditating or practicing progressive muscle relaxation, yoga, or tai chi.
You can work to figure out your own triggers for stress and depressive symptoms and avoid them if possible. Common triggers include:
- An unrealistic workload or a nonstop onslaught of emails and deadlines
- Financial burdens
- Major life changes, such as moving
- Internal fears, attitudes, and beliefs
- Lack of control over situations
Once you know what triggers stress for you, you can develop strategies to cope with it.
By improving your problem-solving skills and working on positive behaviors, you may be able to reduce your stress.
You can also try these tips to proactively manage stress and relieve or prevent your depressive symptoms:
- Get a hobby that relaxes you.
- Say “no” to responsibilities that you don’t want or need, such as extra work projects or other nonessential obligations.
- Take breaks from your routine, such as a vacation.
- Spend time with supportive friends and family.
- Take part in religious services.
- Do breathing exercises to slow your heart rate.
- Avoid situations that trigger stress, depression, or anxiety.
- Avoid alcohol and recreational drugs.
-
Get therapy
Research suggests that short-term therapy can help treat dysthymia.
There are several different types of psychotherapy or talk therapy that may be helpful, including:
- Cognitive-behavioral therapy
- The cognitive-behavioral analysis system of psychotherapy (CBASP)
- Interpersonal psychotherapy (IPT)
- Manualized group therapy
- Problem-solving therapy
- Couples, family or group therapy
- Combination therapies
The type of therapy you may want or need will depend on your personality, goals, and symptoms.
Therapy may help you identify negative thought or behavior patterns and how to change them.
It may also help you cope with triggers of depression, such as stress, loss, isolation, rejection, and other upsetting experiences.
In general, therapy can help you develop skills and strategies for overcoming emotional and psychosocial barriers to good mental health now and in the future.
-
Stay socially engaged
Although you may benefit from avoiding stressful public or social circumstances, such as public speaking or over-commitment to unnecessary activities,
it is important to stay involved in activities with friends, family, and the community. Interacting with others and staying connected to people helps prevent symptoms of depression.
You can get or stay involved in multiple ways:
- Volunteer with a charity, religious organization, or community group that is important to you.
- Take part in social gatherings with friends and neighbors.
- Focus on outings that you find most enjoyable and that make you feel less lonely.
- Take time to work on your most important relationships, for example with your family, spouse, and closest friends.
- Scale back on the number of social media platforms you use to emphasize quality over quantity.
-
Eat to support your mental health
Although diet alone cannot cure dysthymia or depression, it can help reduce inflammation, boost mood, and keep your body healthy so that you can cope better with stress.
A healthy diet can also make it more likely that you achieve remission from depressive symptoms.
The SMILES trial in Australia found that a modified version of the Mediterranean diet plan helped significantly more people achieve remission from depression than people who received social support instead.
If you wish, you can try the modified Mediterranean diet as well using the following number of daily servings for each of these food groups:
- 5–8 servings of whole grains
- 6 servings of vegetables
- 3 servings of fruit
- 2–3 servings of low-fat, unsweetened dairy
- 1 serving of raw, unsalted nuts
- 3 tablespoons of olive oil per day
The plan is called the ModiMed Diet and also includes 3–4 servings of legumes, 2 servings of fish, 3–4 servings of lean red meat, 2–3 of poultry, and up to 6 eggs per week.
The diet also recommends avoidance (or cap at no more than three per week) of refined cereals, fast food, sweetened food, processed meats, alcohol (except red wine with food), and sugary drinks.
Calories and the total quantity of food are not limited to this diet since weight loss is not the goal.
Separate research also supports the use of omega-3 polyunsaturated fatty acids as part of a healthy diet to reduce symptoms of depression.
-
Consider aromatherapy
There is a long history of using essential oils for depression treatment.
Although many oils have been used to relieve symptoms, there is only limited scientific research to date on the therapy.
Modern research may support the use of aromatherapy and massage aromatherapy for relieving symptoms of depression.
- Although some of the included studies were low quality, a review of aromatherapy-related depression studies found that essential oil inhalation or aromatherapy massage may be beneficial for some people with depression.
- In some cases, people experienced less emotional stress and fewer depressive symptoms after inhaling essential oils such as lavender and rose otto.
- Similarly, massage plus aromatherapy relieved depressive symptoms — in some cases more than massage alone
-
- In this study, the most common oils used alone or in combination included lavender and bergamot. Other oils included petitgrain, Yuzu, cedarwood, and rose otto.
- For inhaled aromatherapy, treatments varied from daily to twice per week over a period of a few days to eight weeks.
- For massage, treatments varied from weekly to once every two weeks for up to eight sessions. The effects appeared to increase when there were more, lengthier sessions over a longer period of time.
- In a study of people with depression and arthritis, inhaling a blend of lavender, marjoram, eucalyptus, rosemary, and peppermint essential oils (in a carrier oil) significantly reduced pain and depression.
- In a study of mice with depression-like behavior and stress, inhaling essential oil from Asarum heterotropoides (wild ginger) helped reduce symptoms and improved the levels of mood regulators in the brain.
- According to the authors of the study, lemon oil and lavender oil inhalation have been found to have similar anti-anxiety and anti-depression effects on animals in other studies.
- Inhalation of cinnamon essential oil was found to decrease depression-like behaviors in another study on mice.
In addition to the above studies, many recommendations exist for different essential oils to improve symptoms of depression.
The studies mentioned above and other sources discussing the use of essential oils for depression suggest that these oils may be useful as aromatherapy:
- Bergamot
- Lavender
- Roman chamomile
- Ylang ylang
- Sweet orange
- Grapefruit
- Lemon
- Cinnamon
- Neroli
- Frankincense
- Sandalwood
- Cedarwood
- Jasmine
- Wild ginger
You can inhale the oil directly from the bottle, put a few drops on a cotton ball and inhale, add it to a diffuser, put a few drops in a bath, or dilute it in massage oil and rub it into your skin.
However, if you are normally very sensitive to strong scents or if you have allergies to common carrier oils (such as coconut or almond oil), you should proceed with caution or consider a different therapy.
-
Ask about supplements and herbs
The Mayo Clinic strongly recommends that anyone considering alternative or complementary medicine for depression, including supplements and herbs, should first discuss their options with their physician.
This is because supplements commonly used to treat depression, such as St. John’s wort, can interact with other medications, such as blood thinners, birth control, cancer drugs, antidepressant drugs,g and others.
Before you start or stop any medicine, herb, or supplement to manage your dysthymia symptoms, talk with a health care professional. Some evidence exists supporting the use of:
- St. John’s wort, SAMe and omega-3 fatty acid supplements: A review of dozens of studies examining herbs and supplements for depression symptoms found that St. John’s Wort, SAMe (S-adenosyl methionine), and omega-3 fatty acids all have promising research supporting their effectiveness.
-
- The study reported conflicting results from studies of St. John’s Wort; however, many trials that included people other than those with strict diagnoses of major depressive disorder (such as other types of depression) found positive results for improved mood with doses ranging from about 900 to 1,500 milligrams/day.
- The study found that early research on SAMe may indicate it can be a useful addition to certain antidepressant drugs by boosting response and remission rates. Doses ranged from 200 to 1,600 milligrams/day.
- The study also reported that 20 high-quality trials support the use of omega-3 fatty acid supplements of about five times the standard dietary intake in the U.S.
- Passionflower, kava, L-lysine plus L-arginine, and magnesium: Another review reports promising research supporting passionflower, kava, L-lysine and L-arginine, and magnesium as possible herbal preparations and supplements that may reduce anxiety and insomnia.
- Zinc: A randomized trial found that people with major depression who received a daily 25-milligram zinc supplement in addition to their antidepressant medication had improved symptoms compared to people who received a fake (placebo) supplement. (49)
- Folic acid and vitamin B12: According to one study, low folate and low vitamin B12 levels are associated with depression in humans. The researchers suggest that early research points to the usefulness of these supplements for improving treatment outcome in depression. They suggest doses of 800 micrograms of folic acid per day and 1 milligram/day of vitamin B12 should be studied.
- Traditional Chinese Medicine (TCM): A review of many studies on traditional herbs used in China for the treatment of depression found that the Xiao Yao San formula is the most promising therapy based on existing research.
- However, the researchers found that this preparation was made with different herbal combinations from study to study, so it may be difficult to determine exactly what part of the formula shows promise for depression symptoms.
Precautions
- Do not attempt to self-diagnose dysthymia. It shares symptoms with many types of depression and other personality disorders.
- Get evaluated by a health professional if you believe you may have dysthymia.
- Most people with dysthymia require medication and talk therapy to get better.
- Do not attempt to self-treat. Depression can lead to suicidal thoughts and actions, and a medical treatment plan can help make sure you are receiving the care you need to help avoid severe complications from your condition.
- Do not stop taking your prescribed medication without first talking with your doctor.
- Do not start any herbs, supplements, or alternative therapies for your dysthymia without first consulting a health care professional who is aware of your formal diagnosis and all other medications and supplements you take.
- If you are having thoughts of suicide, tell someone, and seek professional psychiatric or medical care immediately.
Dysthymia Key Points
- Dysthymia is chronic depression. It can last for years and vary in intensity over time. It can also exist at the same time as major depressive episodes.
- There is no known cause for dysthymia and no single effective cure.
- Conventional treatment for this condition usually involves a combination of antidepressant drugs and talk therapy.
- Do not attempt to self-diagnose or self-treat dysthymia, since it can have serious health consequences and may also be easily confused with other mental health problems.
Natural ways to manage your symptoms and even improve dysthymic mood include:
- Exercise.
- Proactively manage your stress.
- Get therapy.
- Stay socially engaged.
- Eat to support your mental health.
- Consider aromatherapy.
- Ask about supplements and herbs.