Experiencing chest pains can be a scary feeling — especially since it’s one of the most common symptoms associated with having a heart attack.
But there’s another heart condition called pericarditis that can cause ongoing chest pains, which are sometimes sharp and can make it difficult to breathe.
Pericarditis (or inflammation of the sac that holds the heart) is found in roughly 5 percent of all patients admitted to the emergency department for chest pain unrelated to a heart attack.
Why is pericarditis dangerous? Because it can cause a buildup of fluid around the heart that stops it from working correctly.
Who’s at the highest risk of developing pericarditis?
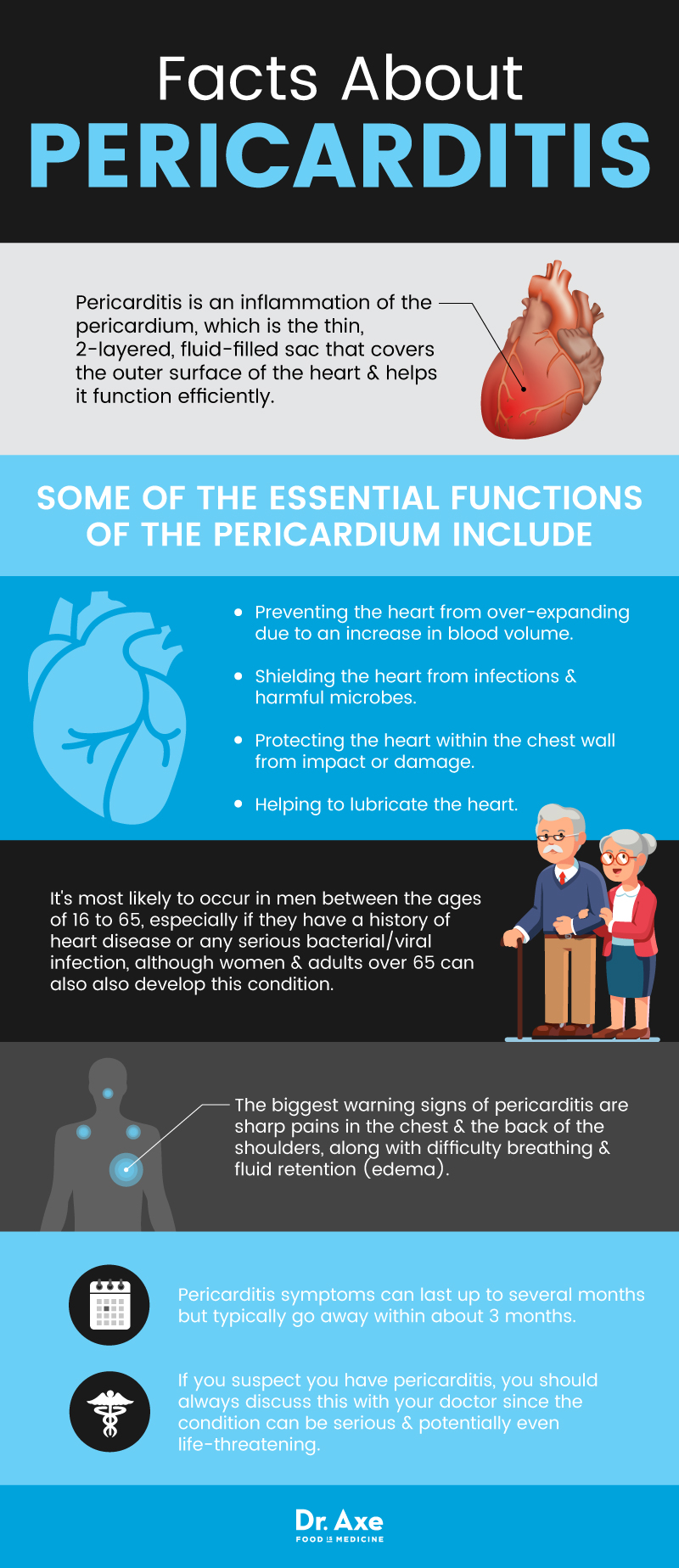
It’s most likely to occur in men between the ages of 16 to 65, especially if they have a history of heart disease or any bacterial severe/viral infection. However, women and adults over 65 can also develop this condition.
The most significant warning signs of pericarditis are sharp pains in the chest and the back of the shoulders, along with difficulty breathing and fluid retention (edema).
If you suspect you have pericarditis, you should always discuss this with your doctor since the condition can be severe and potentially even life-threatening.
Some of the ways you can manage pericarditis symptoms, which you’ll learn much more about below, include:
treating infections, viruses, and autoimmune diseases; resolving nutrient deficiencies; and eating an anti-inflammatory diet.
What Is Pericarditis?
The definition of pericarditis is an inflammation of the pericardium, which is the thin, two-layered, fluid-filled sac that covers the outer surface of the heart and helps it function efficiently.
Like other types of inflammation, pericarditis is caused by the membrane around the heart becoming red, swollen with fluid, irritated, and potentially damaged.
Some of the essential functions of the pericardium include:
- Preventing the heart from over-expanding due to an increase in blood volume.
- Shielding the heart from infections and harmful microbes.
- Protecting the heart within the chest wall from impact or damage.
- Helping to lubricate the heart.
How severe is pericarditis? It depends on the type of pericarditis that you have and how critical the condition is.
If the pericardium is very inflamed and the heart becomes constricted as a result, then there’s a higher chance that severe symptoms will develop.
Chronic pericarditis that can last for many months or even years is a severe condition because it affects blood flow throughout the body.
Signs & Symptoms of Pericarditis
The most common symptoms of pericarditis include:
- Chest pain, which is sometimes painful, sharp, and “stabbing.” Pericarditis pain is due to friction caused when the heart rubs against the inflamed pericardium.
- Pain when coughing, swallowing, lying down, or breathing heavily (such as when exercising). Usually, the pain will decrease when you sit up and lean forward since this puts less pressure on the pericardium.
- Trouble breathing, including when sleeping and lying down. This can increase fatigue and lethargy.
- A dry cough.
- Swelling in your feet, legs, and ankles.
- Sometimes, increased anxiety.
- Some people hear a rubbing or creaking sound coming from their chest/lungs that are caused by rubbing of the inflamed lining of the pericardium. This is most likely to be noticed when you are leaning forward and breathing heavily.
A severe type of pericarditis is called constrictive pericarditis, which occurs when the pericardium hardens and thickens, causing constriction of the heart muscle.
When the heart becomes compressed, it interferes with normal blood flow and can cause blood to back up into places, and it shouldn’t be — such as the lungs, abdomen, and legs. Signs and symptoms of constrictive pericarditis include:
- Abnormal heart rhythm.
- Swelling in the legs and abdomen, which is sometimes severe.
- Shortness of breath.
- Water retention.
- Heart palpitations.
How long does pericarditis last?
Usually, it develops suddenly and may worsen quickly.
Pericarditis symptoms can last up to several months but typically go away within about three months.
Some people will deal with symptoms for years (chronic pericarditis) and experience flare-ups in symptoms from time to time as the inflammation gets better, but then worsens again.
According to the Cleveland Clinic, “About 15-30% of patients with pericarditis have repeat episodes of pericarditis that come and go for many years.”
Is pericarditis life-threatening? It can be if pericardial effusion and cardiac tamponade occur. (5)
- Pericardial effusion refers to fluid buildup in the space between the pericardium and heart.
- This may lead to cardiac tamponade, which is when there’s so much accumulated fluid that it compresses the heart, which is life-threatening and requires immediate drainage of the liquid.
Pericarditis Causes & Risk Factors
What is the leading cause of pericarditis? There isn’t just one cause since many different health conditions can lead to pericarditis (inflammation around the heart) developing.
There are many different types of pericarditis, all of which have different underlying causes and symptoms. The main examples of pericarditis include: (6)
- Acute pericarditis — Develops suddenly and usually lasts several months.
- Chronic pericarditis — lasts for three months or longer.
- Cardiac tamponade — A severe compression of the heart that is considered a medical emergency.
- Constrictive pericarditis — Causes the pericardium to harden, stiffen, and develop scar tissue.
- Infectious pericarditis — Caused by a viral, bacterial, fungal, or parasitic infection.
- Idiopathic pericarditis — Does not have a known cause.
- Traumatic pericarditis — Due to an injury to the chest, impact, trauma, or accident.
- Uremic pericarditis— Due to kidney failure.
In many cases, it’s not known precisely what causes pericarditis, which is referred to as idiopathic pericarditis.
In developed countries, idiopathic pericarditis is responsible for 80 percent to 90 percent of all cases.
Some people develop pericarditis due to having an autoimmune disease, which can cause the body to “attack” its tissue,
causing inflammation around the heart and many other symptoms like joint pain, weakness, and so on.
Some risk factors and underlying causes of pericarditis can include:
- Having had a heart attack, recent heart surgery such as bypass surgery (this is called postpericardiotomy syndrome), radiation therapy, cardiac catheterization, or radiofrequency ablation (RFA).
- Viral infections, most of which affect the gastrointestinal system.
- Bacterial infections, including tuberculosis (TB). The disease is a significant cause of pericarditis in developing countries but is responsible for less than 5 percent of cases in developed countries.
- Fungal infections or those caused by a parasite.
- Certain autoimmune diseases, such as lupus, rheumatoid arthritis, and scleroderma. Having ankylosing spondylitis is another risk factor since this type of arthritis causes abnormal fusions in the spine, inflammation, and pain in the upper body and pelvis.
- Damage or impact to the chest, such as after a car accident.
- Health problems, such as kidney failure or tumors.
- Certain genetic diseases, such as familial Mediterranean fever (FMF).
- In rare cases, they are taking medications that suppress the immune system, such as if treating a health problem like cancer or HIV.
Related: How to Maintain Normal Troponin Levels
Conventional Treatments for Pericarditis
Your doctor can determine a pericarditis diagnosis by performing a physical exam, taking tests, and discussing your symptoms, medical history, and risk factors.
You might need to have some of the following tests done to determine if and how severely your pericardium is inflamed:
- Chest X-rays
- Electrocardiogram (ECG or EKG) to look for changes in your heart rhythm
- Echocardiogram (echo) to check for fluid or pericardial effusion
- Cardiac MRI to check for pericardial inflammation
- CT scan to check for abnormalities around the heart
- Cardiac catheterization to determine if the heart is constricted
- Blood tests to determine the causes of inflammation (such as high C reactive protein levels).
One diagnosis of pericarditis is made; conventional treatments typically include:
- Pain-reducing medications, which can consist of prescription-strength pain-killers or over-the-counter drugs such as ibuprofen, aspirin, or other nonsteroidal anti-inflammatory drugs (NSAIDs). Taking medicines with an anti-inflammatory analgesic for one to two weeks is “the first-line treatment” for acute pericarditis. (8)
- If an infection is a root cause, antibiotics, or antifungal medications.
- An anti-inflammatory drug called colchicine. In the case of chronic or recurrent pericarditis, your doctor may recommend that you take NSAIDs and colchicine for several years to help manage the condition. Colchicine has been shown to help reduce recurrences, which tends to occur in about 30 percent of patients who don’t utilize any type of preventive therapy.
- Diuretics to help control fluid retention, swelling, and edema.
- Sometimes steroids/corticosteroids such as azathioprine, IV human immunoglobulins, or anakinra are used to control inflammation and autoimmune reactions. Some cardiologists believe that corticosteroid use should be limited to patients with NSAID contraindications/intolerance and not used by patients with specific conditions such as autoimmune diseases. (9)
- In severe cases, surgery may need to be performed to protect the heart and drain excess fluid from the pericardium and surrounding area. Pericardiocentesis is a surgery that involves inserting a long, thin catheter to drain the extra liquid. Some people with constrictive pericarditis may need to have part of their pericardium removed (called a pericardiectomy) to prevent further constriction of the heart.
6 Natural Ways to Help Prevent & Manage Pericarditis Recovery
1. Rest & Reduce Stress
Any type of bodily stress, including intense exercise and physical activity beyond walking and stretching, can be harmful during pericarditis.
It’s recommended that you take it easy while you heal, so be sure to get plenty of sleep every night (at least seven to nine hours) and to rest when needed.
Before returning to intense exercise, talk to your doctor about whether it’s safe.
Exercise can be beneficial once you’ve healed enough since it benefits immune function, circulation, and cardiovascular health.
While you’re recovering, try to manage emotional stress by doing stress-relieving activities, including:
meditation, breathing exercises, light yoga or stretching, getting massages, journaling, walking outside, praying, art or creative activities, etc.
2. Eat An Anti-Inflammatory Diet
Support your immune system by cutting out processed foods from your diet and eating whole, nutrient-dense foods that provide antioxidants, vitamins, and minerals.
If you have a health condition such as an autoimmune disease — for example, Hashimoto’s, which causes hypothyroidism — eating an anti-inflammatory diet is critical for improving gut health and immune function.
Here are steps you can take to reduce inflammation by eating a nutrient-dense diet:
- Eat plenty of raw fruits and vegetables. Include foods high in vitamin C and Alike oranges, kale and other leafy greens, kiwi, strawberries, grapefruit, red peppers, green peppers, guava, and broccoli.
- Consume bone broth daily, which is another healing food that will supply essential vitamins and minerals.
- Eat probiotic-rich foods because they boost immune function and replenish the healthy bacteria in your gut. Some excellent options include kefir, cultured vegetables (like sauerkraut and kimchi), kombucha, coconut kefir, and cultured yogurt.
- Eat high-quality protein such as lean grass-fed beef, pastured eggs, organ meats like liver, and wild-caught salmon
- Consume healthy fats like coconut oil, olive oil, grass-fed butter, ghee, avocado, nuts, and seeds.
- Avoid inflammatory foods that can worsen existing health conditions, including processed grains (especially those gaining gluten), conventional dairy products, foods with added sugar and synthetic ingredients, processed meats, fast food, and fried foods.
- Eliminate sources of trans-fatty acids in your diet, such as fast food and processed foods. Avoid refined grains like white bread, white rice, pasta, and refined sugar. Avoid coffee, alcohol, and tobacco products.
- Drink plenty of water throughout the day to help reduce coughs and make it easier to breathe. Try to drink a glass of water every two to three hours for a total of about eight glasses per day.
3. Fight Viruses & Infections
You can use the following natural remedies to protect yourself from viruses, bacterial infections, and fungal infections — which can make pericarditis worse and even be an underlying cause:
- Use oregano oil either topically or internally, which acts as a natural antibacterial agent without causing harmful side effects. Oregano oil also has the power to help treat viral conditions, reduce inflammation, and relieve respiratory symptoms that are caused by allergies.
- Antiviral herbs can help build your body’s defenses against infections and contributing health problems. Those include wormwood, black walnut, oregano essential oil/capsules, garlic, bentonite clay, activated charcoal, and grapefruit seed extracts. Herbs may help treat infections and attack viral pathogens, plus they offer cardiovascular, digestive, and anti-inflammatory support during periods of illness.
- Adaptogenic herbs like Rhodiola (Rhodiola Rosea) and astragalus (Astragalus membranaceous) can be beneficial when it comes to supporting immune health and helping you deal with physical and mental stress or fatigue.
4. Improve Your Ability To Breathe
If you’re experiencing shortness of breath and coughs, use a humidifier in your home, especially when you sleep at night.
A humidifier can help to loosen mucus and relieve wheezing and limited airflow.
Also, be sure to quit smoking if you currently smoke.
Smoking is highly inflammatory and increases the risk of many diseases, including heart disease.
If you do smoke, talk to your doctor about programs and products that can help you quit.
It’s also important to try to avoid secondhand smoke and other lung irritants, such as dust, vapors, fumes, and air pollution.
You can use eucalyptus oil, which contains the constituent called cineole, to reduce shortness of breath while improving respiratory function.
To help reduce airway inflammation, try making a facial steam bath with eucalyptus oil.
Pour a cup of boiling water into a bowl and mix in 10 drops of the oil. Then place a towel over your head as you lean over the bowl and inhale deeply for five to 10 minutes.
5. Reduce Inflammation With Supplements
Certain supplements might help you to heal and feel better while you recover. These include:
- Hawthorne berry (Crataegus oxyacantha L), sometimes called “the heart herb,” has cardio-protective abilities, including helping to prevent conditions that raise the risk for pericarditis, such as angina, high blood pressure, hardening of the arteries, irregular heartbeat, and even congestive heart failure. (11) You can safely take between 160 to 1,800 milligrams per day for a three- to 24-week time period.
- Vitamin C helps to boost your immune system by acting as an antioxidant and fighting free radical damage.
- Omega 3 fatty acids have anti-inflammatory effects and are beneficial for cardiovascular health.
- B vitamins can help give you more energy if you’re feeling fatigued.
- Vitamin D3 helps support the immune system.
- A magnesium supplement can help relax constricted or spasming muscles in your chest. It may also support cardiovascular health and lower feelings of restlessness/anxiety, which can help you get better sleep. (12) Many adults suffer from magnesium deficiency without even knowing it. However, you shouldn’t take magnesium without speaking with your doctor first if you have low blood pressure or kidney disease/kidney failure.
- Probiotics are beneficial for gut health and your immune system.
- N-acetylcysteine helps to decrease the severity and frequency of coughing attacks and improves overall lung function if you have shortness of breath.
6. Try Natural Sleep Aids & Pain-Relievers
If you’re experiencing pain while lying down and have trouble sleeping or relaxing, some of these natural pain-killers may be able to help:
- Peppermint essential oil can be used topically to improve circulation and reduce muscle tension. Lavender oil is useful for promoting relaxation, easing stress, and helping you fall asleep. Try this homemade muscle rub recipe to help alleviate sore muscles, including tightness in your chest.
- Try taking a magnesium-rich Epsom salt bath to soothe joint pain and muscle soreness.
- Apply warm compresses and heating pads or ice packs to your chest and painful areas, which can be helpful for the temporary relief of aches and inflammation.
- Drink bone broth, which contains minerals in forms that your body can easily absorb. It’s a good source of calcium, magnesium, phosphorus, silicon, sulfur, chondroitin sulfate, and glucosamine, which can help to reduce inflammation, arthritis symptoms, and joint pain.
- Visit an acupuncturist or chiropractor for help relieving tightness, anxiety, and other symptoms stemming from dysfunction of the neuromuscular system.
Precautions
If you experience warning signs of pericarditis — exceptionally sharp pain in your chest, back and shoulders, and difficulty breathing — then call your doctor or a cardiologist to schedule an evaluation.
Remember that pericarditis can be deadly if it progresses and is left untreated, so always air on the safe side by having a physical exam performed and talking to your doctor about your risk factors.
Key Points
- Pericarditis is inflammation of the pericardium, which is the thin, two-layered, fluid-filled sac that covers the outer surface of the heart and helps it function efficiently.
- Causes of pericarditis include a history of heart disease, kidney failure, infections, autoimmune responses, or reactions from an injury, surgery, or trauma.
- Symptoms of pericarditis include chest pain, trouble breathing, fluid retention, coughing, pain in the shoulders and back, difficulty laying down or sleeping, and swelling in the abdomen, legs, and feet.
6 Natural Ways to Help Manage Pericarditis Symptoms & Recovery
- Eating an anti-inflammatory diet
- Treating infections
- Getting plenty of rest
- Taking supplements and herbs to boost immunity
- Controlling autoimmune responses
- Treating pain with essential oils, massage, and other natural approaches