Tachycardia
Tachycardia is when the heart beats faster than normal while at rest. It is a change in your heart’s rhythm, and in some cases, it is harmless.
In others, it can lead to serious complications. However, with medical management and some lifestyle changes, many people can avoid the greatest risks of tachycardia.
What Is Tachycardia?
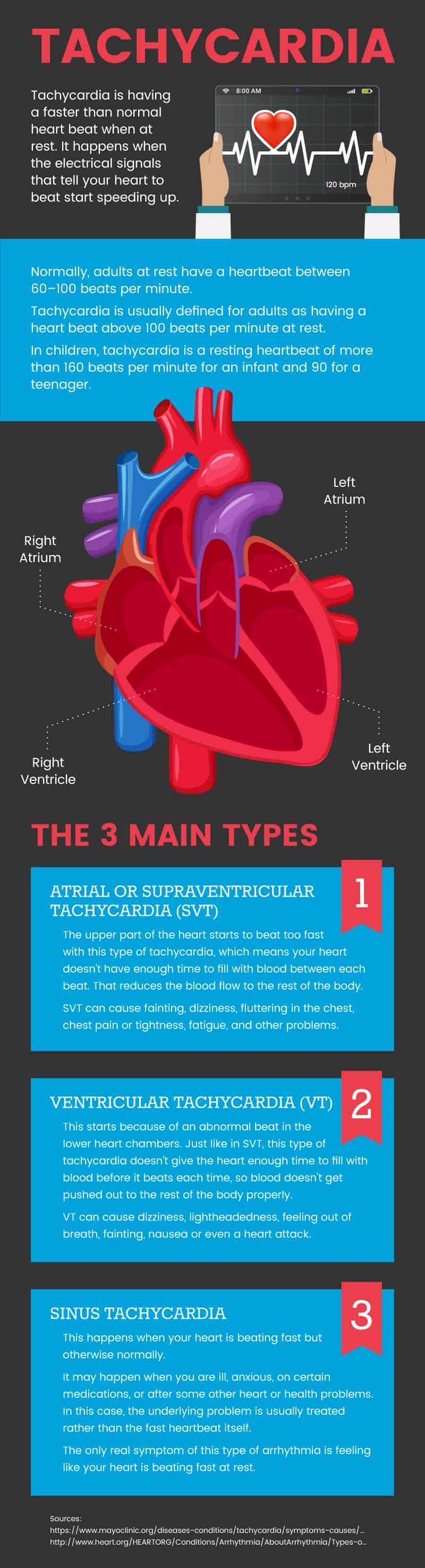
A common disorder of the heart’s rhythm, tachycardia, is having a faster-than-normal heartbeat when at rest.
It happens when the electrical signals that tell your heart to beat start speeding up.
Normally, adults at rest have a heartbeat between 60 and 100 beats per minute.
Tachycardia is usually defined for adults as having a heartbeat above 100 beats per minute at rest.
However, in children, tachycardia is a resting heartbeat of more than 160 beats per minute for an infant and 90 for a teenager.
Tachycardia in children is rare and may be due to problems with the heart developed before they were born. It can also be caused by illness or other health conditions.
The most common type in children is supraventricular tachycardia (SVT); most kids with this problem do not need treatment, but a doctor should evaluate them.
There are several types of tachycardia:
- Atrial fibrillation
- Atrial flutter
- Sinus tachycardia
- Supraventricular tachycardia, or SVT
- Ventricular tachycardia
- Ventricular fibrillation
According to the American Heart Association, tachycardia can be simplified into three main types:
- Atrial or supraventricular tachycardia (SVT)
- This starts because of an abnormal beat in the upper chambers of the heart. Your heart has a natural pacemaker that sends electrical signals to tell your heart to beat. The upper part of the heart starts to beat too fast with this type of tachycardia, which means your heart doesn’t have enough time to fill with blood between each beat. This reduces the blood flow to the rest of the body.
- SVT can cause fainting, dizziness, fluttering in the chest, chest pain or tightness, fatigue, and other problems.
- Ventricular tachycardia (VT)
- This starts because of an abnormal beat in the lower heart chambers. Just like in SVT, this type of tachycardia doesn’t give the heart enough time to fill with blood before it beats each time, so blood doesn’t get pushed out to the rest of the body properly.
- VT can cause dizziness, lightheadedness, feeling out of breath, fainting, nausea, or even a heart attack.
- Sinus tachycardia
- This happens when your heart is beating fast but otherwise normally. It happens when your heart’s natural pacemaker simply sets a faster pace for each heartbeat. It may happen when you are ill, anxious, on certain medications, or after some other heart or health problems. In this case, the underlying problem is usually treated rather than the fast heartbeat itself.
- The only real symptom of this type of arrhythmia is feeling like your heart is beating fast at rest.
Signs & Symptoms
Some people with tachycardia don’t notice any symptoms.
The condition may be discovered by chance during a doctor’s visit.
Other people will know when they are experiencing an episode. Tachycardia symptoms may vary by the type of tachycardia you have.
In general, however, people with tachycardia may have the following signs and symptoms:
- A racing, uncomfortable, or irregular heartbeat
- Feeling short of breath.
- Feeling lightheaded
- Fainting
- Having a fast pulse
- Chest pain
In serious cases or cases where ventricular tachycardia or SVT are untreated, they can cause:
- Heart attacks
- Unconsciousness
- Fatigue
- Damage to the heart muscle
In rare cases, complications may include blood clots, stroke, heart failure, and sudden death.
Causes & Risk Factors
An irregularity causes tachycardia in the electrical signal that makes the heartbeat.
However, there are many root causes of that irregularity. These tachycardia causes include:
- A damaged heart from heart disease
- Heart disease or an abnormality present from birth
- Abnormal electrical signals to the heart present from birth
- Strenuous exercise
- Sudden stress or fright
- Anxiety
- Anemia
- Smoking
- High or low blood pressure
- Drinking too much caffeine or alcohol
- Fever
- Certain medications
- Use of certain street drugs
- Hyperthyroidism and Graves’ disease
- Electrolyte imbalance
Risk factors for tachycardia include any problem that strains the heart or damages its tissue. It can also occur in people with sarcoidosis.
Fast heartbeat is most common in older people or who have a family history of heart rhythm disorders.
Other risk factors for tachycardia are lifestyle-related or medical and can include:
- Smoking
- Heavy alcohol or caffeine use
- Use of street drugs
- Stress or anxiety
- Heart disease
- High blood pressure
- Sleep apnea
- Thyroid problems
- Diabetes
- Anemia
Conventional Treatment
Treatment for your tachycardia will depend on the type of arrhythmia you have.
In some cases, no treatment may be needed.
In others, as in most sinus tachycardia, doctors will treat the underlying problem — such as anemia or fever — and your heartbeat will return to normal.
Typically, conventional treatment for new disease includes:
- Doing special movements, called vagal maneuvers, to try to self-regulate your heartbeat.
- Taking medication, such as a pill or an injection at the hospital
- CPR, in emergency cases where the tachycardia has stopped your heart or is not getting enough blood through
- Shocking your heart (cardioversion) with a paddle system and patches on your chest, using an automated external defibrillator (AED)
In cases where the condition is expected to return, treatment may include:
- Ablation: The abnormal part of your heart that is causing the tachycardia will be destroyed.
- Medication: Anti-arrhythmia pills can be taken regularly to help avoid episodes of tachycardia. Other medications to treat conditions that also affect your heart may be prescribed as well.
- Pacemaker: A small device is implanted under your skin. When it notices your heart is off rhythm, it sends a little electrical pulse to help your heartbeat return normal.
- Implantable cardioverter (ICD): A small device implanted in your chest to monitor your heartbeat. If it detects an abnormal rhythm, it gives electrical shocks to your heart to normalize the heartbeat. This is usually only done in people with ventricular tachycardia, who are at particular risk of sudden death due to arrhythmia.
- Surgery: In some cases, surgery may create a little maze of scar tissue on the heart. This can help stop the abnormal electrical pulses from making the heartbeat too fast because the scar tissue doesn’t let the electricity pass.
Tachycardia: 7 Natural Ways to Manage Symptoms
In some cases, your doctor can show you how to stop tachycardia naturally.
Before you attempt to learn how to slow down tachycardia on your own, however, you should make sure you have been officially diagnosed.
After discussing the cause and best course of treatment for your condition with your physician, you may be able to use certain natural remedies for slowing a rapid heart rate.
In general, natural methods for managing tachycardia symptoms target overall heart health and the prevention of heart disease and known tachycardia triggers.
Natural ways to manage tachycardia and prevent future episodes may include:
- Do vagal maneuvers.
- Exercise and eat a heart-healthy diet.
- Avoid energy drinks and limit alcohol.
- Avoid certain medicines, smoking, and recreational drugs.
- Reduce stress and anxiety.
- Ask about dietary supplements.
- Try acupuncture.
As always, be sure to discuss any changes to your diet or exercise, including the use of supplements and natural remedies, before you try to use them to treat tachycardia.
Some herbs and supplements can cause or worsen tachycardia or cause serious problems for people taking heart medicines or certain health conditions.
You should also tell your doctor about any changes in your symptoms, any worsening of symptoms, or any other health problems you develop.
Go to regular checkups for your heart so that your doctor can keep track of your heart problem over time.
-
Do vagal maneuvers
Vagal maneuvers are just moves that affect your vagal nerve, which helps control your heartbeat. These include:
- Coughing
- Bearing down, as if you have a bowel movement
- Blowing through a syringe
- Immersing your face in cold water
- Putting an ice pack on your face
- Gagging yourself with a tongue depressor
- Carotid massage (gentle, circular massage under the jaw for about 10 seconds)
These actions may help your vagal nerve slow or stop a fast heartbeat.
During an episode, call your doctor if these moves do not stop the fast heartbeat.
-
Exercise and eat a heart-healthy diet
Exercise can help keep your heart healthy and help reduce your risk of conditions leading to tachycardia.
It can also help you maintain a healthy weight, which can reduce your risk of heart disease.
These two simple suggestions are notorious for being easier said than done. Simple ways to add more exercise to your lifestyle include:
- Take the stairs instead of the elevator.
- Park farther away from the entrance to stores.
- Take a walk on your lunch break or after dinner.
- Use a push or walking lawnmower rather than a riding mower.
- Do some spring cleaning; wash windows, scrub the floors, dust, wipe the baseboards down, and do other physically demanding chores.
- Garden.
- Play with your kids or grandkids outside.
To eat a heart-healthy diet, opt for foods low in fat and high in fiber. Avoid foods that are high in fat and calories but low in nutritional value.
More specifically, the American Heart Association suggests you focus on nutrient-rich foods such as:
- Fruits and vegetables
- Whole grains
- Low-fat dairy
- Poultry (fat and skin trimmed off) and fish
- Nuts and legumes
- Healthy fats, such as olive oil or avocados
-
Avoid energy drinks and limit alcohol.
Energy drinks
While it is commonly recommended that people with arrhythmias avoid caffeine, there isn’t clear evidence that caffeine alone causes a faster or irregular heartbeat, even in people who already have tachycardia.
However, energy drinks often combine caffeine, taurine, large doses of vitamins and herbs, sugar, and other chemicals.
There have been numerous reports of people experiencing fast or irregular heartbeats after having one or more energy drinks, particularly when combined with exercise or other stimulating drugs or activities.
Do not drink energy drinks if you have tachycardia.
While it may also be wise to limit your overall caffeine intake, you can discuss with your doctor what may be a healthy amount of coffee or tea for you.
Alcohol
Alcohol is also often fine in moderation for people with known tachycardia problems.
However, binge drinking and regular heavy alcohol use are known to increase people’s risk of tachycardia.
Heavy alcohol use and binge drinking should be avoided if you have been diagnosed with tachycardia or are experiencing a fast heartbeat at rest.
-
Avoid certain medicines, smoking, and recreational drugs.
Everything you put in your body can impact your health and interact with other things you consume.
Avoid smoking and street drugs, and ask a health care professional about all drugs, herbs, supplements, and over-the-counter (OTC) medicines you take to help minimize your risk of tachycardia.
-
Medicines
- Some OTC drugs for coughs and colds have ingredients that can trigger tachycardia.
- Non-prescription diet or weight-loss drugs may contain ingredients, such as caffeine and ephedrine, that can cause tachycardia (as well as other health problems).
- In some cases, even herbal weight loss medications have unregulated or hidden ingredients, such as the chemical appetite suppressant sibutramine, that can cause tachycardia.
- Some of these ingredients may also be in prescription drugs, so be sure that whoever prescribes a weight-loss treatment to you is aware of your risk for tachycardia.
- Ensure that any doctor prescribing medicine to you is aware of your tachycardia since other medications may cause heart arrhythmias or aggravate tachycardia.
-
Smoking
- Smoking increases the risk of tachycardia. Besides, for people already diagnosed with heart trouble, such as mild heart failure, continuing to smoke increases the risk of tachycardia and death.
- People with existing tachycardia and implanted cardioverter defibrillators (ICDs) who still smoke are more likely to have serious complications and to have their ICD shock them inappropriately due to rapid heartbeat than nonsmokers.
- Stop smoking if you have tachycardia.
-
Recreational drugs
- Stimulant street drugs such as cocaine can cause heartbeat irregularities.
- In many cases, this type of tachycardia can be hard to treat. Ask a medical professional for help to recover from addiction to street drugs.
- Misuse of prescription drugs should also be avoided. Some drugs, such as the attention-deficit disorder (ADD) drug Adderall, can increase heart rate and other severe side effects when misused or combined with other drugs.
-
Reduce stress and anxiety
Many people who have issues coping with anxiety or stress have sinus tachycardia or racing heartbeat.
However, many people with other forms of the disease also experience anxiety. Also, tachycardia itself, its potential to happen again, and worries about its impact on your health can all cause anxiety.
No matter which type of tachycardia you have, controlling your stress and anxiety levels may be beneficial.
There are many ways to reduce stress and relieve anxiety. These methods have been shown to reduce anxiety as well as tachycardia:
- Yoga: A review of arrhythmias and natural treatments found that yoga can reduce atrial fibrillation episodes and reduce anxiety and depression.
- Mindfulness-Based Stress Reduction programs: A study of young people with implanted heart devices, postural tachycardia, and other heart problems experienced less stress and anxiety after receiving an intervention involving yoga, meditation, cognitive restructuring (thought therapy), and group support.
- Cognitive-behavioral therapy (CBT): Just three CBT plus exercise sessions resulted in reducing chest pain and sinus tachycardia in a randomized, controlled study. (24) It also reduced depression and fear of bodily sensations (for example, thinking catastrophically about palpitations).
- Aromatherapy: A study of patients who underwent heart surgery found that inhaling lavender essential oil reduced heart rate and blood pressure, which are commonly elevated after surgery due to stress and pain.
-
Ask about dietary supplements.
In some cases, it may be safe and beneficial for you to add supplements to your regimen or to alter your diet to get certain nutrients. These supplements may help reduce the risk of tachycardia or boost heart health.
However, they need to be present in the right amounts. For example, having too much magnesium in your blood can cause other heart problems.
Check with your doctor before beginning anything new, as these supplements may not be appropriate for everyone.
Your doctor should also discuss the right dose with you based on your age, diet, and other medications or supplements.
- Vitamin C: This vitamin is a powerful antioxidant that may improve blood circulation for people with postural tachycardia, prevent atrial fibrillation after surgery, and reduce the likelihood of repeat episodes in people who had persistent atrial fibrillation.
- Magnesium: This mineral has potent anti-arrhythmia effects and is used to prevent tachycardia in heart surgery patients and improve the effectiveness of anti-arrhythmic drugs.
- When taken as a supplement, it is believed to be particularly useful for ventricular tachycardia that doesn’t respond to other therapies.
- With potassium, supplements may be useful for people with deficiencies in preventing serious complications from tachycardia, such as fatal heart attacks.
- Potassium: This mineral has also been used to stop a fast heartbeat after surgery.
- Having a potassium deficiency can cause arrhythmia.
- In one study, potassium supplements were given at the same time as magnesium injections, and together they successfully stopped harmful tachycardia in seven of the eight patients in the study.
- Hawthorn berry: This herb is a traditional treatment for heart rhythm problems such as tachycardia. In one lab study, hawthorn leaf extract reduced the arrhythmia in human heart stem cells.
- According to Dr. Patrick Fratellone of the American Herbalists Guild, dosages of hawthorn used for treating arrhythmias can range from 120 to 240 milligrams twice per day (as a standardized pill), or one or two berries steeped in 8 ounces of water as a tea each day, for three to 24 weeks.
- More research is needed to determine whether calcium, corydalis, valerian, skullcap, and lady’s slipper may be useful as natural remedies for tachycardia.
Although omega-3 fatty acids have frequently been reported as helpful for heart health, some inconsistent research studies suggest it may not be helpful for people with arrhythmias and may even be harmful in some cases.
Talk with your doctor about omega-3 fatty acids before increasing your fatty fish intake or taking a supplement.
Other herbal and supplement options may also be useful for tachycardia.
However, the American Herbalists Guild does not recommend that these all be used in isolation (without conventional medicine) to treat tachycardia. These herbs include:
- Night-blooming Cactus (Cactus Grandiflora’s)
- Scotch broom (Cytisus scoparius)
- Motherwort (Leonurus cardica)
- Lily of the Valley (Convallaria majalis), leaves, and flowers only.
-
Try acupuncture
A review of studies of natural therapies for the treatment of arrhythmias found that acupuncture was safe and effective at reducing recurrences of atrial fibrillation and, in some cases, reducing chest pain and, in several studies, reducing hypertension.
Ask your doctor if you may be a good candidate for acupuncture before seeking this treatment. People with tachycardia brought on by fear of needles should avoid acupuncture.
Precautions
- Always consult a health care professional before starting or stopping a medication, herb, or supplement.
- Do not attempt to diagnose yourself. There are many reasons your heart may seem to beat fast, and tachycardia is impossible to diagnose based on symptoms alone. Knowing the type of rhythm problem you suffer from is critical to getting the right treatment.
- Tachycardia treatment at home should only be done once you know the type of tachycardia you have and after you have discussed treatment with your doctor.
- Tell your doctor if you have any new or worsening symptoms.
- Seek emergency medical care if your irregular heartbeat causes you to faint, have trouble breathing, or causes chest pain for more than a few minutes.
- Avoid supplements and herbs known to cause irregular heartbeats, such as cola nut, ephedra, guarana, and creatine.
Key Points
- Tachycardia is an irregularly fast heartbeat (over 100 beats per minute at rest for an adult).
- It is caused by a misfire of the heart’s electrical signals that tell the heart to beat. This misfire can be triggered by anxiety, illness, heart disease, or an abnormality in the heart’s natural pacemaker.
- In many cases, it does not require treatment or cause health problems. However, certain types of this condition can lead to serious complications and even death if they are not treated.
- Follow the treatment plan given to you by a health care professional to manage your symptoms. Do not start or stop medicines, herbs, or supplements without consulting your doctor.
You may also benefit from trying these natural ways to manage symptoms and prevent future episodes:
- Do vagal maneuvers
- Exercise and eat a heart-healthy diet
- Avoid energy drinks and limit alcohol.
- Avoid certain medicines, smoking, and recreational drugs.
- Reduce stress and anxiety
- Ask about dietary supplements.
- Try acupuncture